When IBD Symptoms Hide in Plain Sight on Darker Skin
Picture this: You’re in your doctor’s office, pointing to a spot on your skin that’s been bothering you for weeks. You know something’s wrong—it’s painful, it looks different, and your gut is telling you it’s connected to your IBD. But your doctor glances at it and moves on, not recognizing what you’re seeing. For many people of color in our IBD community, this frustrating scenario plays out far too often when skin complications arise.
This disconnect isn’t about bad doctors or lack of caring—it’s about a gap in medical education and research that’s finally getting the attention it deserves. When textbooks and training materials primarily show how IBD-related skin issues appear on lighter skin, healthcare providers can miss the same conditions when they present differently on darker skin tones.
Summary of Understanding IBD Complications on Skin of Color
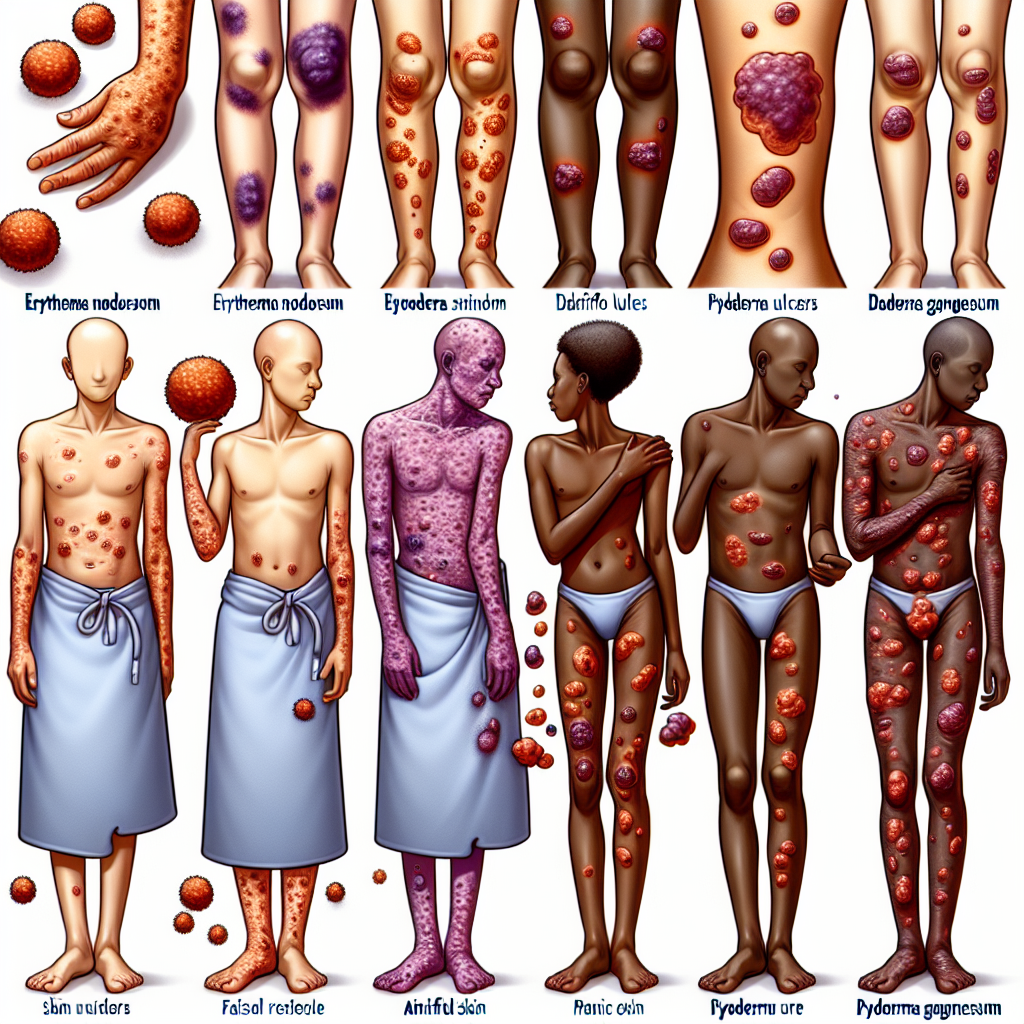
IBD can cause various skin complications, including erythema nodosum (painful red bumps) and pyoderma gangrenosum (deep, painful sores). These conditions are well-documented in medical literature, but there’s a significant problem: most research and clinical examples have historically focused on how these complications appear on lighter skin.
The challenge is that inflammatory skin conditions can look quite different on darker skin tones. What appears as obvious redness on pale skin might present as darker patches, purple discoloration, or subtle changes that are easily overlooked on skin of color. As more African American and Southeast Asian individuals are diagnosed with IBD, this knowledge gap becomes increasingly problematic.
Medical professionals may miss or misdiagnose these skin complications simply because they haven’t been trained to recognize the varied presentations across different skin tones. This can lead to delayed treatment, prolonged suffering, and potentially serious complications that could have been prevented with earlier intervention.
This post summarizes reporting from Understanding IBD Complications on Skin of Color. Our analysis represents IBD Movement’s perspective and is intended to help patients understand how this news may affect them. Read the original article for complete details.
What This Means for the IBD Community
This issue touches on something much deeper than medical textbooks—it’s about feeling seen and heard in healthcare spaces. For our community members with darker skin tones, advocating for proper care becomes an additional burden on top of managing a chronic illness. It shouldn’t be this way, but understanding the reality helps us navigate it better.
If you’re a person of color living with IBD, this information validates what you might have already experienced. That frustrating doctor’s visit where your concerns were dismissed? The skin issue that took months to get properly diagnosed? These experiences are unfortunately common, but they’re not acceptable, and they’re certainly not in your head.
For all IBD patients and their families, this highlights why we need to be proactive advocates for comprehensive care. When we understand the limitations in current medical training, we can better prepare for appointments and push for the attention our symptoms deserve.
Here are some practical steps our community can take:
- Document everything: Take clear photos of any skin changes, noting when they appeared and any associated symptoms. This creates a visual record that can’t be dismissed.
- Seek specialists: If your primary gastroenterologist seems unfamiliar with skin manifestations of IBD, ask for a referral to a dermatologist who specializes in inflammatory conditions.
- Bring research: Don’t hesitate to print relevant studies or articles about IBD skin complications in people of color to share with your healthcare team.
- Trust your instincts: If something feels wrong with your skin, keep pushing for answers. You know your body better than anyone else.
The broader implications extend beyond individual patient care. This knowledge gap reflects systemic issues in medical research and education that affect multiple conditions, not just IBD. When clinical trials and medical studies lack diversity, the resulting treatments and diagnostic criteria may not work equally well for everyone.
However, change is happening. Medical schools are increasingly recognizing the need for more diverse representation in their curricula. Dermatology programs are expanding their focus to include skin conditions across all ethnicities. Research initiatives are specifically seeking to understand how various conditions present in different populations.
For our IBD community, this evolution in medical understanding offers hope for better care in the future. But it also means we need to stay informed and continue advocating for ourselves and each other in the present.
Consider discussing these questions with your healthcare team:
- How familiar are you with IBD skin complications in patients with darker skin tones?
- What should I watch for regarding skin changes related to my IBD?
- If I develop skin issues, who should I see first—you or a dermatologist?
- Are there any clinical trials or research studies I should know about?
This issue also connects to broader trends we’re seeing in IBD research. There’s growing recognition that IBD affects diverse populations differently—not just in skin manifestations, but in disease progression, treatment response, and overall outcomes. The medical community is slowly but surely working to address these disparities through more inclusive research and targeted interventions.
The Path Forward
While we can’t change decades of limited research overnight, we can work together to ensure that everyone in our IBD community receives the comprehensive care they deserve. This means continuing to share our experiences, supporting each other through healthcare challenges, and celebrating the progress being made in medical education and research.
The conversation about healthcare disparities isn’t always comfortable, but it’s necessary. By acknowledging these gaps openly, we create space for solutions to emerge. Every time a patient advocates for better care, every time a doctor takes the initiative to learn about diverse presentations of IBD, every time researchers include diverse populations in their studies—these actions collectively push medicine forward.
Remember that your experience and your voice matter. If you’ve faced challenges getting skin complications properly diagnosed or treated, sharing your story can help others in similar situations. Whether through support groups, online communities, or conversations with healthcare providers, your perspective contributes to the growing awareness around this issue.
IBD Movement provides information for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.







