When Your Battle Is Invisible: Understanding Life With IBD
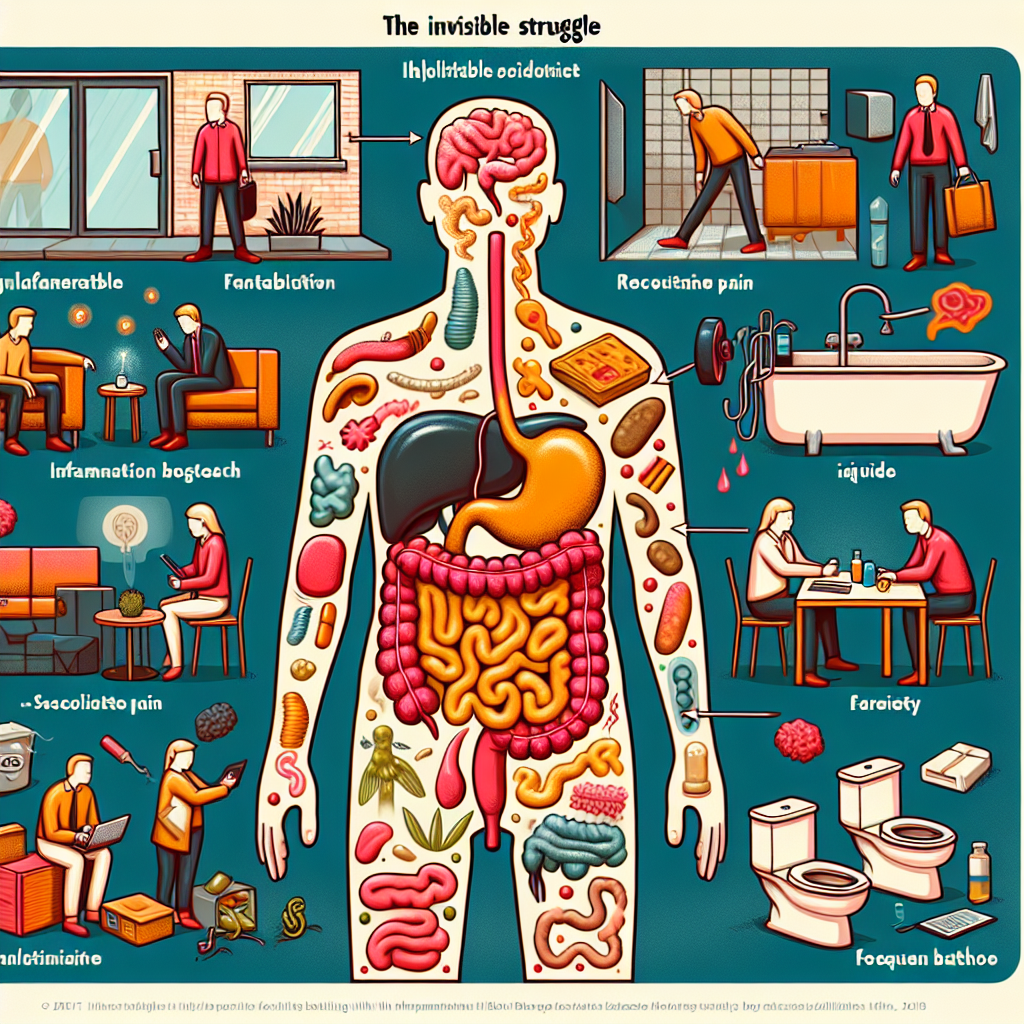
You wake up in the morning and no one can see the exhaustion etched into your bones. Your coworkers don’t notice the careful calculations you make about bathroom locations, or the way you strategically plan your meals around your body’s unpredictable responses. To the outside world, you might look perfectly healthy—but inside, you’re fighting a daily battle that most people can’t begin to understand. This is the reality for millions living with inflammatory bowel disease, where the most challenging aspects of the condition often remain hidden from view.
If you’ve ever felt frustrated by well-meaning comments like “but you don’t look sick,” or struggled to explain why you need to cancel plans last minute, you’re not alone. The invisible nature of IBD creates unique challenges that go far beyond the physical symptoms, touching every aspect of how we navigate relationships, work, and daily life.
Summary of Read the original article here
A recent News24 article brings important attention to inflammatory bowel disease, highlighting how this invisible illness affects millions worldwide. The piece explains that IBD encompasses both Crohn’s disease and ulcerative colitis—conditions that cause long-term inflammation in the digestive tract, leading to symptoms like chronic pain, fatigue, frequent bathroom visits, and unpredictable flare-ups.
The article emphasizes the challenging nature of IBD symptoms, which can include recurring diarrhea, abdominal pain, weight loss, and exhaustion. What makes IBD particularly difficult is its unpredictable pattern of flares and remissions, making it hard for patients to plan their daily activities, work schedules, or social commitments.
Regarding causes, experts note that while the exact triggers aren’t fully understood, IBD likely results from a combination of genetic factors, immune system dysfunction, and environmental influences. The article suggests that lifestyle factors such as stress, diet, and early antibiotic use might also contribute to disease development.
The piece highlights the psychological impact of living with IBD, noting that anxiety, depression, and isolation are common experiences, particularly because the illness is often invisible to others. For diagnosis, the article explains that doctors typically use a combination of physical exams, lab tests, endoscopy, and imaging scans.
Treatment options discussed include anti-inflammatory medications, immune suppressors, and biologic therapies, with surgery sometimes necessary for complications. The article emphasizes that comprehensive care now includes psychological support, nutritional guidance, and strong support networks alongside medical treatment.
This post summarizes reporting from Read the original article here. Our analysis represents IBD Movement’s perspective and is intended to help patients understand how this news may affect them. Read the original article for complete details.
What This Means for the IBD Community
This article’s focus on the “invisible” nature of IBD resonates deeply with something many of us experience daily—the constant need to advocate for ourselves in a world that doesn’t always understand chronic illness. When mainstream media takes the time to explain the hidden struggles of IBD, it creates opportunities for broader understanding and empathy from our families, friends, and colleagues.
One particularly important aspect highlighted in the article is the unpredictability of IBD. This isn’t just a medical fact—it’s a lived reality that affects how we approach everything from career planning to relationships. The article’s mention of flares and remissions speaks to something many of us know intimately: the challenge of explaining to others why you might feel great one day and terrible the next, sometimes within the same afternoon.
The psychological impact discussed in the article deserves special attention. The isolation that comes with invisible illness is real and significant. When people can’t see your struggle, they may inadvertently minimize it. Comments like “at least it’s not cancer” or “you’re lucky you don’t look sick” can be well-intentioned but deeply hurtful. This article’s acknowledgment of anxiety and depression as common experiences validates what many in our community face.
From a practical standpoint, the article’s emphasis on early diagnosis is crucial. Many of us remember the relief—mixed with anxiety—of finally having a name for what we were experiencing. The diagnostic process described, involving multiple tests and procedures, reflects the reality that IBD diagnosis often requires patience and persistence from both patients and healthcare providers.
Questions to Consider for Your Next Doctor’s Visit
This article raises several important points that might be worth discussing with your healthcare team:
- If you’re experiencing new or worsening symptoms, how can you best communicate their impact on your daily life, not just their medical presentation?
- Are there aspects of your psychological well-being that you haven’t discussed with your doctor? Mental health support is increasingly recognized as a crucial part of IBD care.
- If you’re struggling with the unpredictability of symptoms, what strategies might help you better manage work, school, or family commitments?
- Have you considered connecting with other IBD patients or support groups to help combat the isolation that often comes with invisible illness?
The article’s mention of comprehensive care is particularly encouraging. The shift toward treating the whole person—not just the disease—reflects a growing understanding that IBD affects every aspect of our lives. This includes recognition that nutritional support, mental health care, and strong support networks are just as important as medication in managing the condition effectively.
The Broader Context of IBD Awareness
What’s especially valuable about articles like this one is how they contribute to changing public perception of chronic illness. Every time IBD is discussed in mainstream media with nuance and empathy, it helps chip away at misconceptions and stigma. This matters not just for current patients, but for people who might be experiencing symptoms and don’t yet realize they could have IBD.
The article’s emphasis on seeking medical attention for persistent digestive symptoms could genuinely help someone reading it recognize their own experience and seek appropriate care. Early diagnosis and treatment can significantly impact long-term outcomes, making this kind of awareness crucial.
Furthermore, the article’s discussion of treatment advances offers hope. While we may not have a cure yet, the mention of biologics and comprehensive care approaches reflects the real progress being made in IBD treatment. For newly diagnosed patients or those struggling with current treatments, this perspective can provide much-needed optimism.
The workplace and educational accommodations mentioned in the article are increasingly important as awareness grows. More employers and schools are beginning to understand that invisible disabilities require support, even if that support looks different from accommodations for visible conditions.
Articles like this one serve as powerful tools for advocacy and education. They help us explain our condition to others, validate our experiences, and demonstrate that we’re part of a larger community facing similar challenges. When we share these resources with family members, friends, or colleagues, we’re not just providing information—we’re fostering understanding and empathy.
The focus on breaking silence around invisible illness is particularly powerful. Too often, we feel pressure to hide our struggles or minimize our symptoms to make others comfortable. Articles that encourage openness and understanding create space for more honest conversations about living with chronic illness.
This article also underscores an important truth: living with IBD requires developing a unique kind of resilience. We learn to navigate uncertainty, advocate for our needs, and find strength in community. While these aren’t skills we would have chosen to develop, they often become sources of personal growth and connection with others facing similar challenges.
The emphasis on living “full, productive lives” with proper support resonates deeply. This isn’t about pretending IBD doesn’t affect us—it’s about recognizing that with the right care, understanding, and support systems, we can pursue our goals and maintain meaningful relationships despite the challenges.
For those of us who have been living with IBD for years, articles like this remind us how far awareness has come. For those newly diagnosed or still seeking answers, they provide hope and validation that your experiences are real, recognized, and treatable.
As our understanding of IBD continues to evolve, articles that bridge the gap between medical knowledge and lived experience become increasingly valuable. They help ensure that progress in treatment and awareness translates into real improvements in quality of life for people in our community.
The invisible nature of IBD will always present unique challenges, but increased awareness and understanding—like what this article provides—help ensure that invisible doesn’t mean unsupported. Every conversation started, every misconception corrected, and every person who feels a little less alone because of articles like this one represents progress toward a more understanding and accommodating world for people living with IBD.
IBD Movement provides information for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.







