Beyond Symptoms: The Hidden Anxiety That Haunts IBD Remission
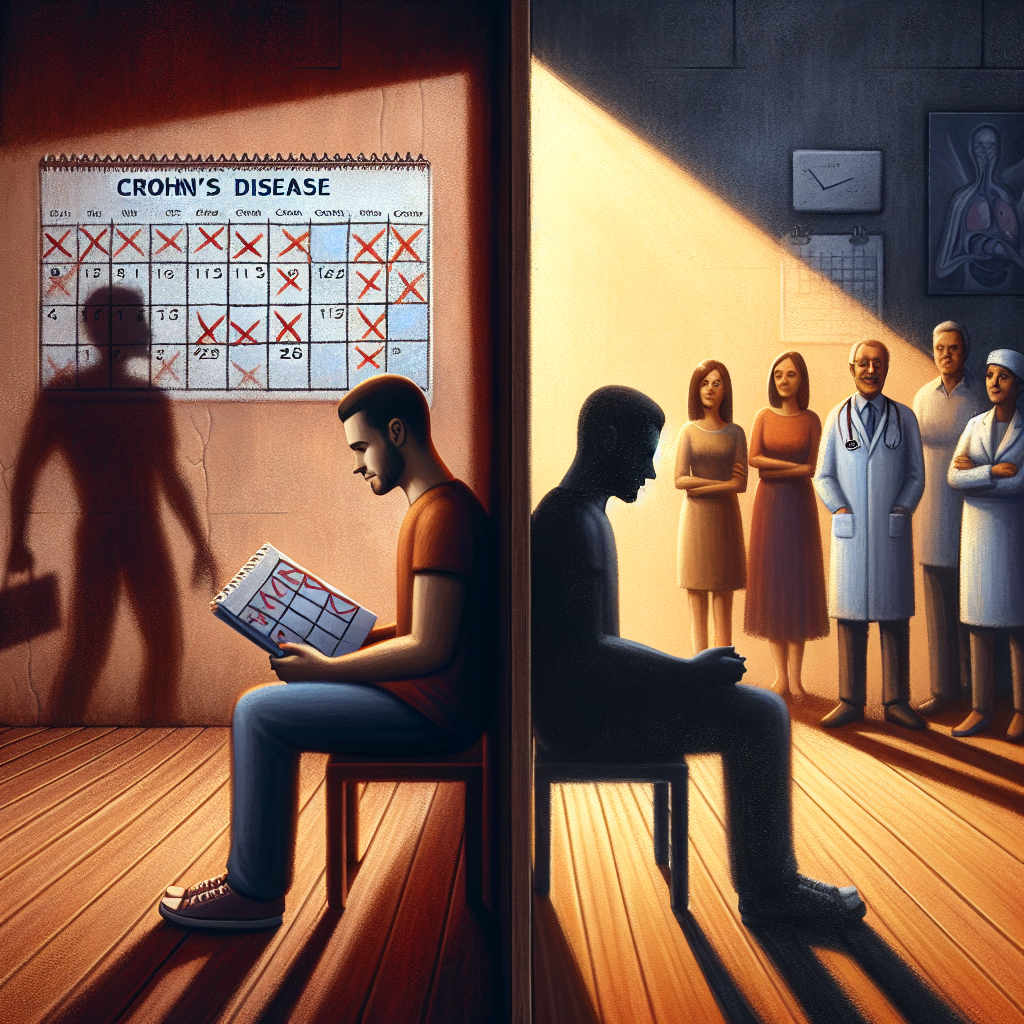
You’re finally feeling good. Your energy is back, your symptoms have quieted, and for the first time in months, you can make dinner plans without that familiar knot of worry in your stomach. But then it creeps in—that whisper of doubt that asks, “How long will this last?” If you’re living with Crohn’s disease or ulcerative colitis, you know this feeling all too well. It’s the shadow that follows even our brightest days.
This isn’t just about physical symptoms—it’s about the mental and emotional toll of living with uncertainty. Even when our bodies cooperate, our minds often remain on high alert, scanning for the first sign that our hard-won remission might be slipping away. It’s a burden that the IBD community knows intimately but doesn’t always talk about openly.
Summary of https://www.healthcentral.com/condition/crohns-disease/worry-about-flaring-even-in-remission
A recent article explores the psychological reality many people with Crohn’s disease face: persistent anxiety about future flare-ups, even during periods of remission. This fear doesn’t disappear with good test results or positive doctor visits. Instead, many find themselves constantly bracing for the next setback, wondering if symptoms will return before an important event, vacation, or milestone.
The piece highlights how this anticipatory anxiety affects daily decisions. People may avoid making plans, decline social invitations, or restrict their diets unnecessarily—all in an attempt to prevent a flare-up that may never come. The unpredictable nature of triggers makes it difficult to trust one’s own body, leading to significant life modifications based on “what if” scenarios.
The article suggests several coping strategies, including open communication with healthcare providers about these psychological concerns, seeking mental health support through therapy or mindfulness techniques, and building strong support networks. The key message is that while worry about future flare-ups is natural, it’s possible to reclaim joy and live more fully despite chronic uncertainty.
This post summarizes reporting from https://www.healthcentral.com/condition/crohns-disease/worry-about-flaring-even-in-remission. Our analysis represents IBD Movement’s perspective and is intended to help patients understand how this news may affect them. Read the original article for complete details.
What This Means for the IBD Community
This article touches on something we rarely discuss in doctor’s offices but desperately need to address: the psychological aftermath of achieving remission. While we celebrate the absence of symptoms, we often ignore the presence of fear that lingers in the background. This isn’t weakness or overthinking—it’s a natural response to living with an unpredictable chronic illness.
What strikes me most about this topic is how it reveals a fundamental gap in IBD care. We have sophisticated tools to monitor inflammation, adjust medications, and track biomarkers, but we’re still learning how to heal the emotional wounds that IBD creates. The fear of flare-ups represents a form of medical trauma—our bodies have broken our trust before, so why should we believe they won’t do it again?
This anxiety manifests differently for everyone in our community. Some people become hypervigilant about every twinge or change in bowel habits, interpreting normal bodily functions as warning signs. Others swing in the opposite direction, ignoring genuine symptoms because they’re so tired of being sick. Many fall somewhere in between, caught in an exhausting cycle of hope and dread.
The ripple effects extend far beyond our individual experiences. Partners, family members, and friends often share this anxiety, walking on eggshells around us or struggling to understand why we can’t simply enjoy feeling good. Children of parents with IBD may develop their own health anxieties, having witnessed firsthand how quickly things can change.
From a practical standpoint, this fear-based decision-making can actually harm our long-term health outcomes. When we avoid activities, restrict our diets unnecessarily, or decline social opportunities, we may be trading short-term peace of mind for long-term isolation and depression. The stress of constant worry can itself trigger flare-ups, creating the very outcome we’re trying to prevent.
Questions to Consider for Your Next Appointment
This research suggests several important conversations to have with your healthcare team:
- How can we distinguish between rational caution and anxiety-driven hypervigilance about symptoms?
- What role might mental health support play in my overall IBD management plan?
- Are there specific lifestyle modifications that are evidence-based versus those driven by fear?
- How can we set realistic expectations for remission that acknowledge both hope and uncertainty?
The Broader Context of IBD Mental Health
This article connects to a growing recognition that IBD is fundamentally a whole-person condition. The medical community is beginning to understand that achieving biochemical remission isn’t enough if patients remain trapped by fear and anxiety. Some IBD centers are now incorporating mental health professionals into their teams, acknowledging that psychological well-being is essential to long-term success.
The timing of this conversation is particularly relevant as we see more people achieving deeper, longer remissions with newer therapies. Paradoxically, having more to lose—more good days, more normalcy—can make the fear of flare-ups even more acute. Success in IBD treatment brings its own psychological challenges that we’re only beginning to understand and address.
What gives me hope is seeing more people in our community speak openly about these fears. Online support groups, social media platforms, and patient advocacy organizations are creating spaces where we can acknowledge that feeling good physically doesn’t automatically mean feeling good emotionally. This transparency is the first step toward healing both aspects of our experience.
The path forward isn’t about eliminating all worry—that would be neither realistic nor necessarily healthy. Instead, it’s about learning to hold space for both hope and uncertainty, joy and caution. It’s about building resilience that allows us to engage fully with life while remaining prepared for challenges that may come.
Moving Forward Together
Remember that seeking help for the emotional aspects of IBD isn’t separate from managing your physical health—it’s an integral part of it. Whether that’s through therapy, support groups, mindfulness practices, or simply honest conversations with loved ones, addressing the psychological impact of IBD is as important as taking your medications or following your treatment plan.
You deserve to enjoy your good days without the constant shadow of “what if.” While we can’t eliminate uncertainty from chronic illness, we can learn to dance with it rather than be paralyzed by it. Your remission—however long it lasts—is worth celebrating, worth trusting, and worth living fully within.
IBD Movement provides information for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.







