Scientists Uncover Why Fistulas Form—Hope for Crohn’s Patients
If you’ve ever lived with the fear of developing fistulas—or are currently managing one—you know the unique anxiety it brings. It’s not just the physical pain, though that’s certainly real. It’s the way fistulas can make you feel like your own body is betraying you, creating connections where none should exist. For too long, we’ve accepted fistulas as one of Crohn’s most unpredictable and devastating complications, something that just “happens” without much understanding of why.
But what if we could finally understand the cellular blueprint behind this complication? What if researchers could pinpoint exactly what goes wrong at the microscopic level when fistulas begin to form?
Summary of https://medicalxpress.com/news/2025-11-scientists-cells-crohn-disease-fistulas.html
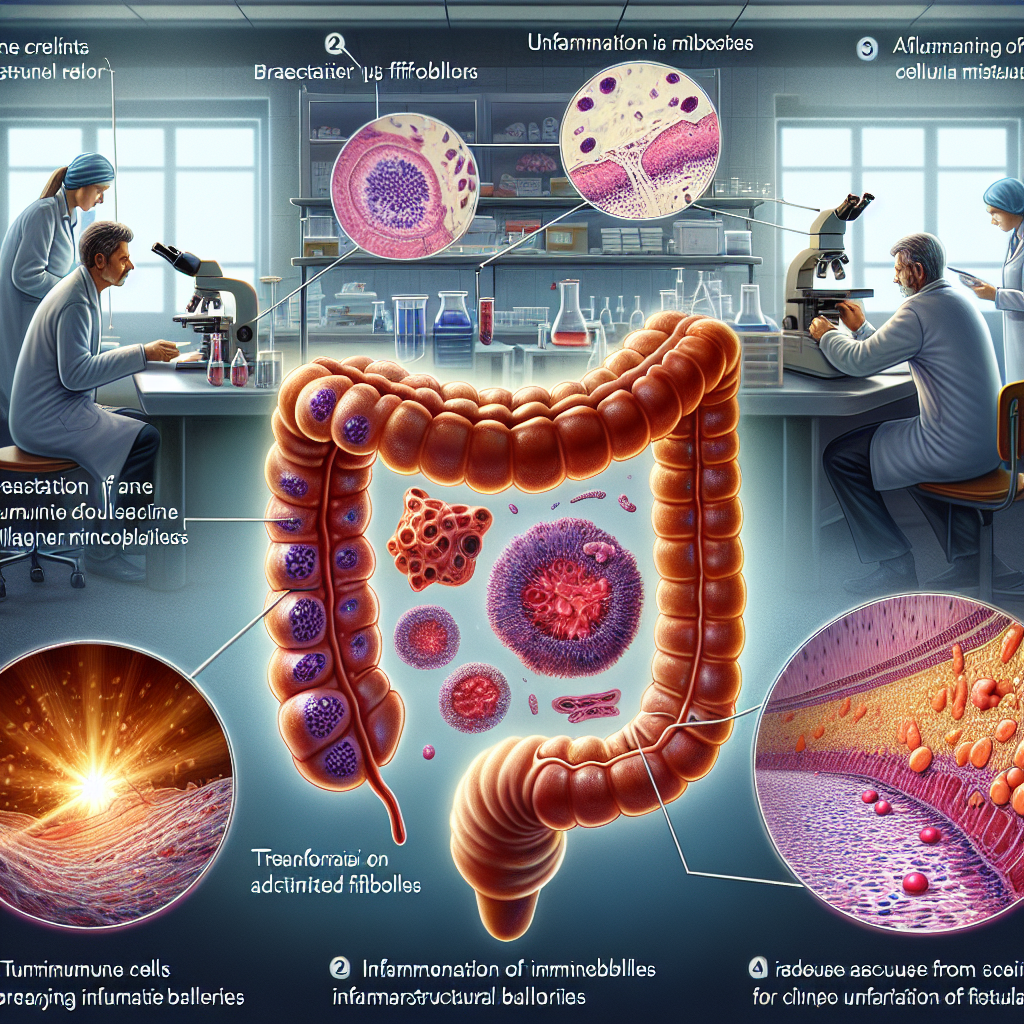
Researchers at the University Hospital of Zürich have made a significant breakthrough in understanding why fistulas develop in people with Crohn’s disease. Their study, published in Science Translational Medicine, focused on examining tissue samples from Crohn’s patients to understand what happens at the cellular level when fistulas form.
The researchers discovered that special cells called fibroblasts play a crucial role in fistula formation. In healthy intestines, these cells help maintain the structural integrity of tissue. However, in people with Crohn’s disease, these fibroblasts become “activated” and start behaving abnormally. Instead of protecting tissue structure, they begin producing substances that actually break down the barriers in the intestinal wall.
The study revealed that this cellular misbehavior is triggered by signals from immune cells and inflammatory molecules that are overactive in Crohn’s disease. When fibroblasts receive these inflammatory signals, they start producing enzymes and proteins that degrade tissue, creating pathways where fistulas can develop over time.
This discovery is significant because it provides a potential target for future treatments. By focusing on these problematic fibroblasts or blocking the signals that activate them, researchers believe it may be possible to prevent fistulas from forming or treat existing ones more effectively.
This post summarizes reporting from https://medicalxpress.com/news/2025-11-scientists-cells-crohn-disease-fistulas.html. Our analysis represents IBD Movement’s perspective and is intended to help patients understand how this news may affect them. Read the original article for complete details.
What This Means for the IBD Community
This research represents a fundamental shift in how we understand fistulas—from mysterious complications to predictable cellular processes. For those of us living with Crohn’s disease, this kind of mechanistic understanding is incredibly powerful because it transforms fistulas from something that “just happens” to something with identifiable, potentially treatable causes.
The identification of fibroblasts as key players is particularly exciting because these cells are already well-studied in other medical contexts. Researchers understand how to target fibroblasts in conditions like cancer and wound healing, which means there’s already a foundation of knowledge to build upon. This could potentially accelerate the development of fistula-specific treatments.
From a practical standpoint, this research validates what many patients have suspected: that fistulas aren’t random occurrences but are connected to the same inflammatory processes driving other Crohn’s symptoms. This means that patients who achieve better overall inflammation control might also be reducing their fistula risk, even if we can’t measure that directly yet.
For patients currently managing fistulas, this research offers hope that future treatments might be more targeted and effective than current approaches. Instead of broad immunosuppression or surgical interventions, we might see therapies that specifically address the cellular mechanisms causing fistula formation.
Questions to Consider Discussing with Your Doctor
This research opens up several important conversations you might want to have with your healthcare team:
- How well-controlled is my current inflammation, and could better control reduce my fistula risk?
- Are there any early signs or biomarkers that might predict fistula development?
- How might this research influence treatment decisions if I develop a fistula in the future?
- Should patients with a history of fistulas be monitored differently?
The Broader Context of IBD Research
This study fits into a larger trend in IBD research toward precision medicine—understanding not just what happens in inflammatory bowel disease, but why it happens and how it varies between individuals. We’re seeing similar mechanistic research in areas like stricture formation, extraintestinal manifestations, and treatment response prediction.
What’s particularly encouraging is that this research was conducted using actual tissue samples from people with Crohn’s disease, not just laboratory models. This means the findings are more likely to translate into real-world treatments that work for actual patients dealing with these complications.
The focus on fibroblasts also connects to broader research into the role of structural cells in IBD. We’re learning that IBD isn’t just about immune system dysfunction—it also involves the cells that form the physical structure of our intestines. This more complete picture of disease mechanisms is leading to more comprehensive treatment approaches.
Managing Expectations and Hope
While this research is genuinely exciting, it’s important to maintain realistic expectations about timelines. Moving from understanding cellular mechanisms to developing and testing new treatments typically takes years, sometimes decades. However, the fact that fibroblasts are already therapeutic targets in other diseases could potentially speed this process.
For patients currently dealing with fistulas, this research doesn’t change immediate management strategies, but it does provide hope that future options may be more effective and less invasive than current approaches. It also reinforces the importance of working closely with experienced IBD specialists who stay current with emerging research.
The psychological impact of understanding “why” shouldn’t be underestimated either. Many patients find that having a scientific explanation for their symptoms reduces anxiety and helps them feel more in control of their condition, even when immediate treatment options remain limited.
This breakthrough reminds us why continued investment in IBD research is so crucial. Every piece of the puzzle we uncover brings us closer to more effective treatments and, ultimately, better quality of life for people living with Crohn’s disease and ulcerative colitis.
The road from laboratory discovery to bedside treatment is long, but research like this provides the foundation for tomorrow’s breakthroughs. For a community that has lived too long with unpredictable complications like fistulas, understanding the cellular mechanisms behind these problems represents genuine progress toward a future where we can prevent them altogether.
IBD Movement provides information for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.