Stanford Study Reveals How ‘Creeping Fat’ Worsens Crohn’s Disease: What This Breakthrough Means for Your Treatment
Summary of Stanford Medicine
IBD Movement provides news analysis and insights for the IBD community. Always consult your healthcare provider for personal medical advice.
A Personal Discovery That Could Change Your Care
If you’re living with Crohn’s disease, you’ve likely experienced the frustration of unpredictable flares and the constant search for better treatments. Today, we’re diving into groundbreaking research from Stanford Medicine that sheds new light on a mysterious aspect of Crohn’s disease that many patients have never heard of: “creeping fat.” This discovery isn’t just another scientific finding—it could fundamentally change how we understand and treat your condition, offering new hope for more targeted therapies and better outcomes.
For years, gastroenterologists have observed this phenomenon during surgeries, but its role in disease progression remained unclear. Now, thanks to this Stanford-led research, we’re beginning to understand how this fatty tissue might be making your Crohn’s symptoms worse and what that means for your future care.
What Stanford Medicine Discovered
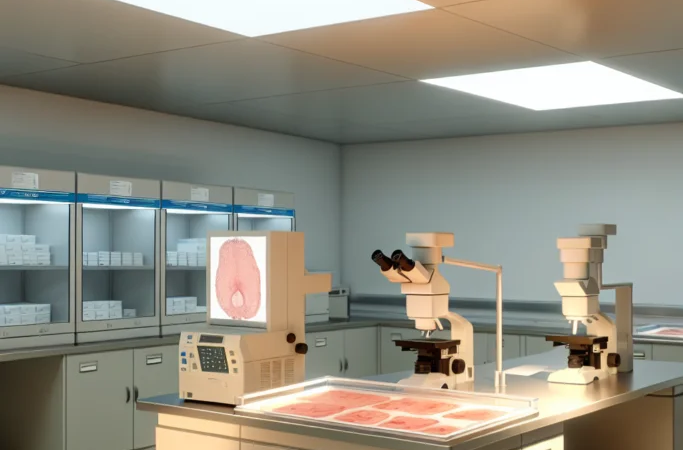
According to Stanford Medicine, researchers have identified a crucial connection between “creeping fat”—abnormal fatty tissue that wraps around inflamed intestinal segments—and the worsening of Crohn’s disease symptoms. This comprehensive study, published in a leading medical journal, represents the first definitive evidence linking this mysterious tissue to disease progression.
The research team, led by Stanford gastroenterologists, analyzed tissue samples from patients with Crohn’s disease who underwent surgical resection. What they found was remarkable: the creeping fat wasn’t just a passive bystander but an active participant in the inflammatory process. According to Stanford Medicine’s findings, this fatty tissue produces inflammatory molecules that can perpetuate and intensify the immune system’s attack on healthy intestinal tissue.
The study revealed that patients with more extensive creeping fat showed higher levels of inflammatory markers and experienced more severe disease courses.
“This fatty tissue isn’t just sitting there—it’s actively contributing to inflammation and making the disease worse,”
researchers noted in their findings. The Stanford team used advanced imaging techniques and molecular analysis to track how this tissue develops and spreads, providing unprecedented insights into its role in Crohn’s disease progression.
As reported by Stanford Medicine, the research also identified specific cellular pathways through which creeping fat influences inflammation, potentially opening doors for targeted therapeutic interventions. The study followed patients over several years, documenting how the presence and extent of this fatty tissue correlated with treatment responses and long-term outcomes.
Understanding the Implications for Your Crohn’s Journey
This discovery represents a paradigm shift in how we understand Crohn’s disease, and the implications for patients like you are profound. For decades, the medical community has focused primarily on intestinal inflammation as the main driver of Crohn’s symptoms. Now, we’re learning that the fat tissue surrounding your inflamed intestines might be acting as a secondary engine of inflammation, potentially explaining why some treatments work better for certain patients than others.
If you’ve ever wondered why your Crohn’s symptoms seem more severe than expected based on your intestinal inflammation alone, creeping fat might provide the answer. This research suggests that traditional approaches to monitoring disease activity—which primarily focus on the intestinal lining—might be missing a crucial piece of the puzzle. The fatty tissue surrounding your inflamed areas could be silently contributing to your symptoms, making flares more intense and recovery more difficult.
This finding also helps explain the variability in treatment responses among people with Crohn’s disease. If you’ve experienced frustration with treatments that work well for others but don’t seem as effective for you, the presence of creeping fat could be a contributing factor. Some patients might have more extensive fatty tissue involvement, requiring different therapeutic approaches to achieve optimal results.
The research opens up entirely new avenues for personalized medicine in IBD care. In the future, your gastroenterologist might be able to assess the extent of creeping fat through advanced imaging techniques, allowing for more tailored treatment plans. This could mean the difference between struggling with persistent symptoms and achieving better long-term remission.
Furthermore, this discovery challenges us to think differently about surgical decisions in Crohn’s disease. When surgery becomes necessary, understanding the role of creeping fat could influence surgical techniques and post-operative care strategies. Surgeons might need to consider not just removing inflamed intestinal tissue but also addressing the surrounding fatty tissue to prevent disease recurrence.
The psychological impact of this research shouldn’t be underestimated either. Many people with Crohn’s disease blame themselves for flares or feel like they’re not managing their condition well enough. Understanding that there’s an additional biological factor—creeping fat—contributing to disease severity can provide validation and reduce self-blame. Your symptoms aren’t just “in your head” or due to poor self-management; there’s a measurable, biological reason why your disease might be more challenging to control.
This research also highlights the importance of comprehensive monitoring and follow-up care. If creeping fat plays a significant role in disease progression, regular assessment of its presence and extent could become a standard part of Crohn’s disease management. This might involve new imaging protocols or biomarker testing to track changes over time.
What Medical Experts Are Saying
Gastroenterologists across the country are calling this research a game-changer for IBD care. The medical community has long recognized that Crohn’s disease involves complex interactions between genetics, immune function, and environmental factors, but the role of fatty tissue has been largely overlooked.
Leading IBD specialists emphasize that this discovery doesn’t change immediate treatment recommendations but provides a foundation for developing new therapeutic targets. When discussing this research with your healthcare team, consider asking about imaging studies that might reveal the extent of fatty tissue involvement in your specific case. Your doctor might also want to discuss how this finding could influence your long-term treatment strategy, particularly if you’ve had difficulty achieving sustained remission with current therapies.
Experts stress the importance of not making treatment changes based solely on this research, as clinical applications are still being developed. However, this finding reinforces the value of working with experienced IBD specialists who stay current with emerging research and can help you understand how new discoveries might eventually impact your care.
Practical Implications for Your IBD Management
- Enhanced monitoring discussions: Ask your gastroenterologist about advanced imaging techniques that might help assess fatty tissue involvement in your disease
- Treatment optimization: This research may explain why certain anti-inflammatory treatments work better for some patients, potentially leading to more personalized therapy selection
- Surgical planning: If surgery becomes necessary, understanding creeping fat’s role could influence surgical approaches and improve long-term outcomes
- Future clinical trials: Stay informed about emerging treatments that specifically target the inflammatory pathways identified in this research
- Comprehensive care approach: Consider this finding as additional validation for the importance of multidisciplinary IBD care that addresses all aspects of your condition
Looking Forward: Hope on the Horizon
This Stanford Medicine study represents more than just an academic discovery—it’s a beacon of hope for everyone living with Crohn’s disease. By identifying creeping fat as an active contributor to disease progression, researchers have opened new pathways for treatment development that could lead to more effective therapies and better quality of life.
The beauty of this research lies in its potential to transform how we approach Crohn’s disease management. Instead of treating symptoms reactively, we might soon be able to target the underlying mechanisms that drive disease progression, including the inflammatory activity of fatty tissue. This could mean fewer flares, better treatment responses, and improved long-term outcomes for patients like you.
As we continue to unravel the complexities of IBD, discoveries like this remind us that every piece of the puzzle matters. Your journey with Crohn’s disease is unique, and research like this brings us closer to truly personalized medicine that addresses all aspects of your condition. Share this news with your healthcare team, connect with fellow IBD warriors in our community, and remember that each scientific breakthrough brings us one step closer to better treatments and, ultimately, a cure.
Source: This post summarizes reporting from Stanford Medicine. Read the original article.







