Your Gut’s Secret Healing Network Could Transform IBD Treatment
Every person with IBD knows that moment when your body feels like it’s turned against you—when inflammation strikes without warning and leaves you wondering if healing is even possible. But what if I told you that deep within your gut, there’s already a sophisticated healing network quietly working on your behalf?
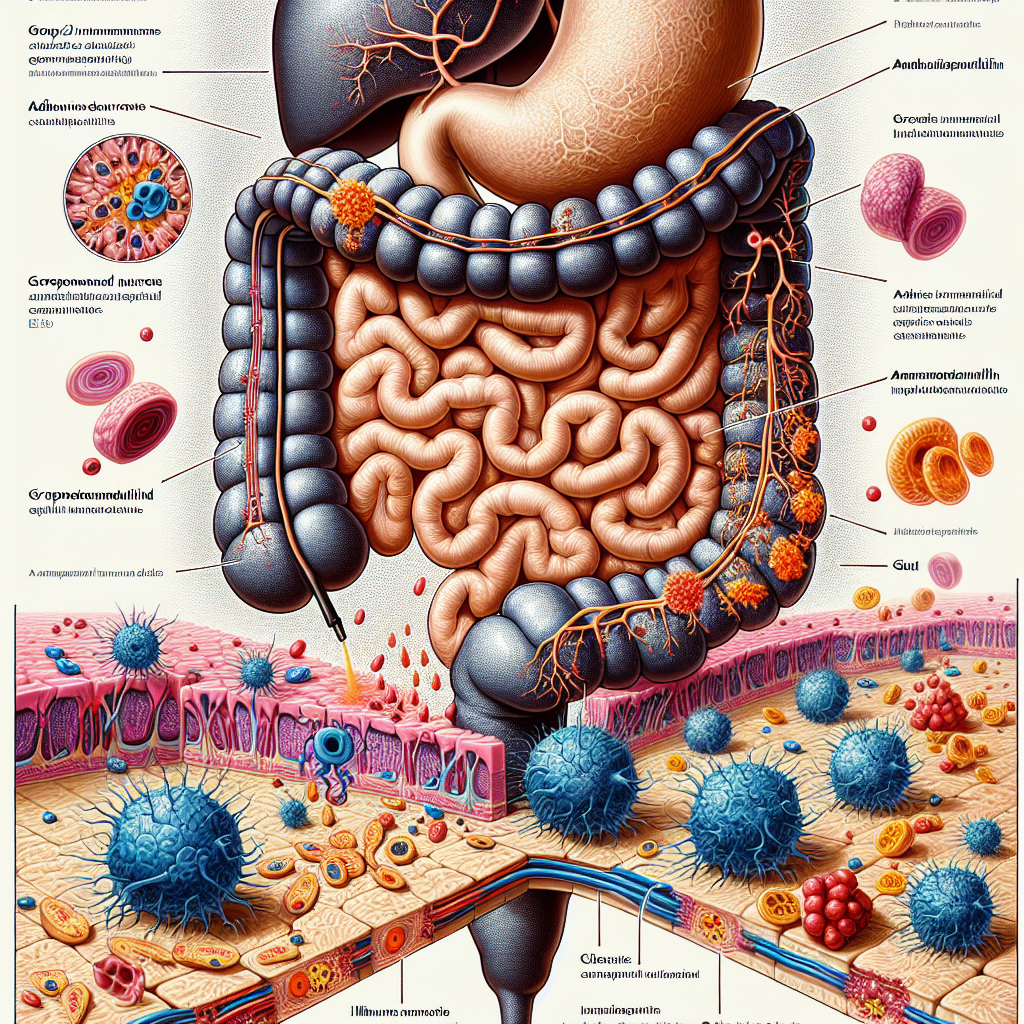
For too long, we’ve thought of IBD as a simple story of inflammation running wild. Yet emerging research reveals something far more hopeful: our intestinal “second brain”—the complex network of neurons lining our gut—isn’t just managing digestion. It’s actively coordinating an intricate dance with our immune system to protect and repair damaged tissue.
Summary of Technology Networks
Recent groundbreaking research has uncovered that neurons in our gut produce a molecule called adrenomedullin 2 (AM2). This isn’t just another protein floating around—it’s a key player in maintaining populations of immune cells that are crucial for tissue repair and healing. The study reveals that these gut neurons don’t just passively respond to inflammation; they actively coordinate immune responses to protect intestinal tissue.
Scientists found that when gut neurons release AM2, it helps sustain specific immune cells that work to calm inflammation and promote healing. This represents a fundamental shift in how we understand the relationship between our nervous system and immune system in the context of IBD. Rather than these systems working independently or even against each other, they’re collaborating in ways we’re just beginning to appreciate.
This post summarizes reporting from Technology Networks. Our analysis represents IBD Movement’s perspective and is intended to help patients understand how this news may affect them. Read the original article for complete details.
What This Means for the IBD Community
This discovery represents more than just interesting science—it’s a potential paradigm shift that could fundamentally change how we approach IBD treatment. For years, most IBD therapies have focused on suppressing our overactive immune systems, essentially telling our bodies to “calm down” without addressing the underlying communication breakdown.
What’s revolutionary about this research is that it suggests we might be able to work with our body’s natural healing mechanisms rather than simply overriding them. Instead of just dampening immune responses, future treatments might enhance the gut’s own ability to coordinate healing through these neural-immune partnerships.
This could be particularly meaningful for those of us who’ve felt frustrated by the “trial and error” nature of current IBD treatments. Many patients cycle through multiple medications, each with their own side effects and limitations, searching for something that truly addresses the root cause of their symptoms. Understanding how gut neurons naturally regulate immune responses opens doors to more targeted, personalized approaches.
From a practical standpoint, this research also validates what many IBD patients have long suspected: that stress, anxiety, and mental health significantly impact gut inflammation. The gut-brain axis isn’t just a metaphor—it’s a literal biological highway where neurons are actively managing immune responses. This means that mind-body approaches to IBD management, from meditation to stress reduction techniques, may have more scientific backing than ever before.
For caregivers and family members, this research offers a new lens for understanding IBD. It’s not just about managing a “broken” immune system—it’s about supporting a complex, interconnected network of systems that are trying to maintain balance and promote healing.
Consider discussing with your healthcare team how this emerging understanding of neuro-immune interactions might inform your treatment approach. Questions might include: How does stress management fit into your overall IBD strategy? Are there ways to support your gut’s natural healing mechanisms alongside conventional treatments? What role might emerging therapies targeting neural-immune communication play in your future care?
This research also connects to broader trends we’re seeing in IBD treatment development. There’s growing recognition that successful IBD management isn’t just about controlling inflammation—it’s about restoring the complex ecosystem of the gut, including the intricate relationships between neurons, immune cells, and the microbiome. We’re moving toward more holistic approaches that address IBD as a systems-level disorder rather than simply an inflammatory condition.
The timing of this discovery is particularly hopeful given the current landscape of IBD research. We’re seeing unprecedented investment in understanding the gut-brain axis, advances in personalized medicine, and growing appreciation for the role of the nervous system in immune regulation. This research adds another crucial piece to that puzzle.
From my perspective, what’s most exciting about this discovery is how it reframes our relationship with our own bodies. Instead of seeing IBD as evidence that our bodies have “failed” us, this research suggests our bodies are constantly working toward healing—we just need to better understand and support those natural processes.
This doesn’t mean we should abandon current treatments or expect miracle cures overnight. But it does suggest that the future of IBD treatment may be more sophisticated, more personalized, and more aligned with our bodies’ natural healing wisdom than ever before.
The research also highlights why integrated care approaches—combining gastroenterology with neurology, psychology, and other specialties—are becoming increasingly important in IBD management. Our guts truly are connected to everything else, and our treatment approaches need to reflect that reality.
Looking Forward
While we’re still years away from treatments based directly on this research, the implications are profound. We may be moving toward a future where IBD therapies work by enhancing our gut’s natural ability to coordinate healing responses, rather than simply suppressing inflammation. For anyone who’s ever felt like their body was working against them, this research offers a different narrative: your gut is already equipped with sophisticated healing mechanisms, and science is getting better at supporting them.
This discovery reminds us that even in the midst of IBD’s challenges, our bodies are constantly working toward balance and healing. Understanding and supporting that process may well be the key to more effective, more personalized IBD treatment in the years to come.
IBD Movement provides information for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.







