Rare Crohn’s Complications: Why We Need to Talk About Complex Cases
Living with Crohn’s disease means accepting that your body can surprise you—and not always in pleasant ways. While most of us focus on managing the daily challenges of inflammation, pain, and unpredictable symptoms, there’s a side of IBD that rarely gets discussed: the truly rare complications that can emerge when this complex disease decides to venture beyond the digestive tract.
Recently, I came across a medical case that stopped me in my tracks—not because it’s common, but because it represents the kind of curve ball that Crohn’s can throw when inflammation refuses to stay contained. It’s a reminder that understanding our disease means acknowledging all its possibilities, even the ones we hope we’ll never face.
Summary of Read more here
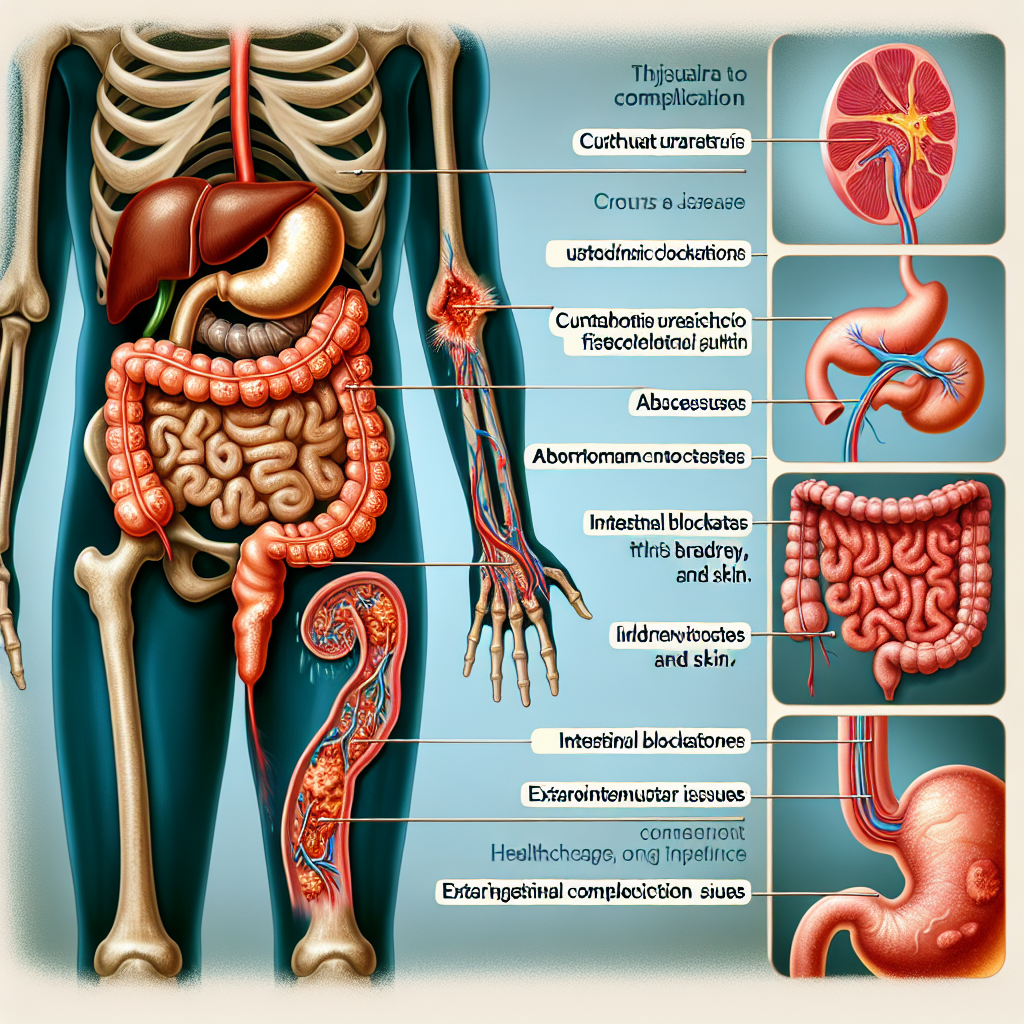
Medical researchers documented an extremely rare case involving a patient with Crohn’s disease who developed what’s called a cutaneous urachovesicoenteric fistula. In simple terms, this means abnormal pathways formed connecting the intestine, bladder, and skin—creating openings where none should exist. This type of complex fistula represents one of the most unusual complications that can occur when Crohn’s inflammation creates connections between different parts of the body. The case highlights how Crohn’s disease can sometimes manifest in ways that challenge even experienced medical teams, requiring specialized surgical intervention and careful coordination between different medical specialties.
This post summarizes reporting from Read more here. Our analysis represents IBD Movement’s perspective and is intended to help patients understand how this news may affect them. Read the original article for complete details.
What This Means for the IBD Community
Before anyone panics, let me be crystal clear: this type of complication is extraordinarily rare. The reason it made it into a medical journal is precisely because doctors don’t see cases like this very often. However, there are several important lessons we can draw from understanding these complex scenarios.
First, this case underscores why Crohn’s disease is classified as a systemic inflammatory condition, not just a digestive disorder. While most of us experience Crohn’s primarily through intestinal symptoms, the underlying inflammation can potentially affect multiple body systems. This is why comprehensive care involves monitoring beyond just your GI tract.
Second, it highlights the critical importance of not dismissing unusual symptoms. In my years of connecting with the IBD community, I’ve heard countless stories of patients whose concerns were initially brushed off as “just part of Crohn’s.” While most symptoms are indeed straightforward manifestations of our disease, complex cases like this remind us that persistent, unusual symptoms deserve thorough investigation.
From a practical standpoint, this case demonstrates why building a strong relationship with your gastroenterologist matters so much. When rare complications do occur, having a doctor who knows your history intimately and can coordinate with other specialists becomes invaluable. The patient in this case likely required input from gastroenterologists, urologists, and surgeons—a team approach that works best when there’s clear communication and leadership.
For caregivers and family members, cases like this illustrate why Crohn’s can feel so overwhelming to those supporting someone with IBD. The unpredictability isn’t just about flare-ups and remissions; it’s about the potential for complications that require specialized knowledge and care. This is why patient advocacy and staying informed about your condition remains so crucial.
Questions to Consider Discussing with Your Doctor
While rare complications like this shouldn’t keep you awake at night, they do provide a framework for important conversations with your healthcare team:
- What warning signs should I watch for that might indicate fistula development?
- How often should we be monitoring for complications beyond standard IBD symptoms?
- If I develop unusual symptoms, what’s the best way to communicate urgency to your office?
- Do you have established relationships with other specialists who understand IBD complications?
- What preventive measures can we take to minimize my risk of complex complications?
These questions aren’t meant to create anxiety, but rather to ensure you’re prepared and your medical team is thinking comprehensively about your care.
The Broader Context of IBD Complexity
This case also connects to broader trends we’re seeing in IBD care. As our understanding of inflammatory bowel diseases becomes more sophisticated, we’re recognizing that successful management requires looking at the whole person, not just the affected organ. This is why modern IBD care increasingly involves multidisciplinary teams and why patient education focuses on understanding the systemic nature of these conditions.
The fact that rare cases like this get documented and published serves our community in important ways. It helps train the next generation of doctors to recognize unusual presentations, contributes to our collective knowledge about what’s possible with IBD, and reminds the medical community that inflammatory bowel diseases can be far more complex than textbook descriptions suggest.
More personally, reading about cases like this reinforces something I’ve learned through years of living with IBD: the importance of trusting your instincts about your body. While we can’t predict or prevent every possible complication, we can commit to being informed, engaged patients who advocate for thorough care when something doesn’t feel right.
For those of us managing Crohn’s day by day, it’s worth remembering that knowledge is power, even when that knowledge involves scenarios we hope never to face. Understanding the full spectrum of what’s possible with our condition helps us make informed decisions about treatment, builds our confidence in medical conversations, and reminds us why consistent, quality care matters so much.
The bottom line is that while Crohn’s disease can surprise us, we’re not powerless against those surprises. Building strong medical relationships, staying informed about our condition, and maintaining open communication about symptoms—even unusual ones—gives us the best chance of navigating whatever complications might arise. Cases like this remind us that rare doesn’t mean impossible, but it also doesn’t mean inevitable. Most importantly, it reinforces that when complex situations do occur, there are medical teams equipped to handle them, and documented cases help ensure that knowledge is shared and preserved for future patients who might need it.







