New Research Links Red Meat to IBD Risk – What It Means for You
There’s something deeply personal about standing in the grocery store meat section when you have IBD. Every package feels like a question mark—will this help me heal, or could it be quietly working against me? If you’ve ever wondered whether your favorite steak dinner might be contributing to your symptoms, you’re not alone in that concern.
The relationship between what we eat and how our gut responds has never been more clear, and new research is shedding light on how red meat specifically might be affecting those of us in the IBD community. It’s the kind of discovery that makes you pause and really think about the choices we make three times a day.
Summary of Original article
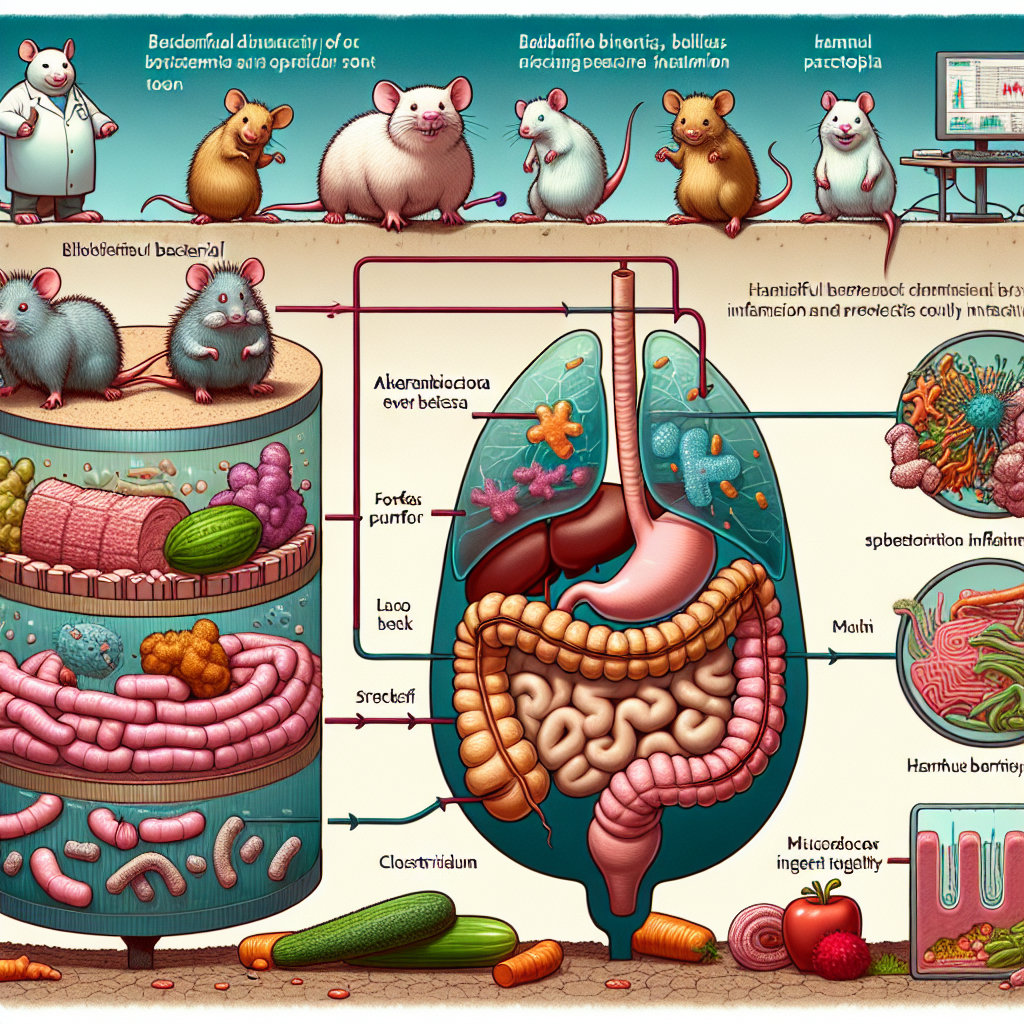
Recent research has revealed concerning connections between red meat consumption and inflammatory bowel disease development. In laboratory studies, mice fed diets high in red meat experienced significant disruptions to their gut microbiome—the delicate ecosystem of bacteria that helps keep our digestive system healthy.
The study found that red meat diets led to a breakdown of the protective gut lining, allowing harmful bacteria to flourish while beneficial bacteria declined. This bacterial imbalance triggered increased inflammation throughout the digestive tract, creating conditions that could worsen existing IBD symptoms or potentially contribute to disease development.
The research suggests that the inflammatory effects aren’t just temporary—they appear to create lasting changes in the gut environment that could have long-term implications for digestive health. These findings add to a growing body of evidence linking red meat consumption to various inflammatory conditions.
This post summarizes reporting from Original article. Our analysis represents IBD Movement’s perspective and is intended to help patients understand how this news may affect them. Read the original article for complete details.
What This Means for the IBD Community
As someone who’s spent years helping people navigate life with IBD, this research hits close to home because it validates what many patients have been experiencing firsthand. I’ve heard countless stories from community members who noticed their symptoms improving when they reduced red meat intake, even before science caught up to explain why.
What’s particularly significant about these findings is how they help us understand the mechanism behind what many of us have observed. It’s not just that red meat might trigger symptoms—this research suggests it may actually be reshaping our gut microbiome in ways that promote the kind of chronic inflammation that drives IBD.
For those currently managing Crohn’s disease or ulcerative colitis, this information raises important questions about dietary strategy. While we know IBD is complex and no single food causes the disease, understanding how certain foods might tip the scales toward inflammation gives us more tools for self-advocacy.
The gut lining breakdown mentioned in the study is particularly relevant for our community. Many of us already struggle with intestinal permeability—often called “leaky gut”—and knowing that red meat consumption might worsen this condition could explain why some people feel better when they modify their protein sources.
From a practical standpoint, this doesn’t mean you need to swear off red meat forever if it’s something you enjoy and tolerate well. But it does suggest that being mindful about frequency and portion sizes might be worth considering, especially during flare periods when your gut is already under stress.
I’m also thinking about the families and caregivers in our community who are constantly trying to figure out how to best support their loved ones with IBD. This research provides another piece of the puzzle for meal planning and grocery shopping decisions. It’s not about creating fear around food, but rather empowering informed choices.
The timing of this research is particularly interesting given the growing focus on personalized nutrition in IBD care. While some people in our community thrive on carnivorous diets, others find plant-based approaches more healing. This study might help explain why individual responses to red meat can vary so dramatically.
One thing I want to emphasize is how this connects to broader themes we’re seeing in IBD research. There’s an increasing recognition that the foods we eat don’t just provide calories—they’re actively communicating with our gut bacteria and immune system. Every meal is essentially a conversation with your microbiome.
For those who are newly diagnosed or still figuring out their trigger foods, this research might provide a starting point for experimentation. Consider keeping a food and symptom journal while gradually reducing red meat intake to see if you notice any patterns. Remember, what works for one person may not work for another, but having this information helps you make more informed decisions.
Questions worth discussing with your gastroenterologist include: How might your current red meat intake be affecting your specific IBD subtype? Are there certain preparation methods or cuts that might be less inflammatory? Should you consider working with a registered dietitian who specializes in IBD to develop an eating plan that accounts for these findings?
I also think this research underscores the importance of looking at our overall dietary patterns rather than fixating on individual foods. The Mediterranean diet, which emphasizes fish and plant proteins over red meat, has shown promise for IBD management, and these findings might help explain part of that benefit.
Moving Forward with Hope and Practical Wisdom
Here’s what I want you to take away from this: knowledge is power, but it doesn’t have to create anxiety around every bite. This research gives us another tool for understanding how we can support our gut health, but it’s just one piece of the larger IBD management puzzle.
If you currently eat a lot of red meat and are concerned about these findings, consider this an opportunity for gentle experimentation rather than dramatic overnight changes. Try incorporating more fish, poultry, legumes, or plant-based proteins into your rotation. Pay attention to how your body responds, and remember that small, sustainable changes often create the most lasting benefits for those of us managing chronic conditions.
IBD Movement provides information for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.







