How Social Connection Transforms Life with Crohn’s Disease
There’s a moment that stays with me from my early days with Crohn’s disease—sitting in a busy restaurant, watching people around me enjoy their meals without a second thought, while I calculated every bite and worried about the nearest restroom. I felt utterly alone, even surrounded by friends. That feeling of invisible isolation is something many of us with IBD know intimately, but what I’ve discovered since then is how profoundly the right kind of support can reshape not just our experience with the disease, but our entire quality of life.
The power of connection in chronic illness isn’t just about having someone to talk to—it’s about having different types of support that meet us exactly where we are in our journey. Whether we’re navigating a devastating flare, celebrating remission, or somewhere in between, the social networks we build become as essential to our wellbeing as any medication we take.
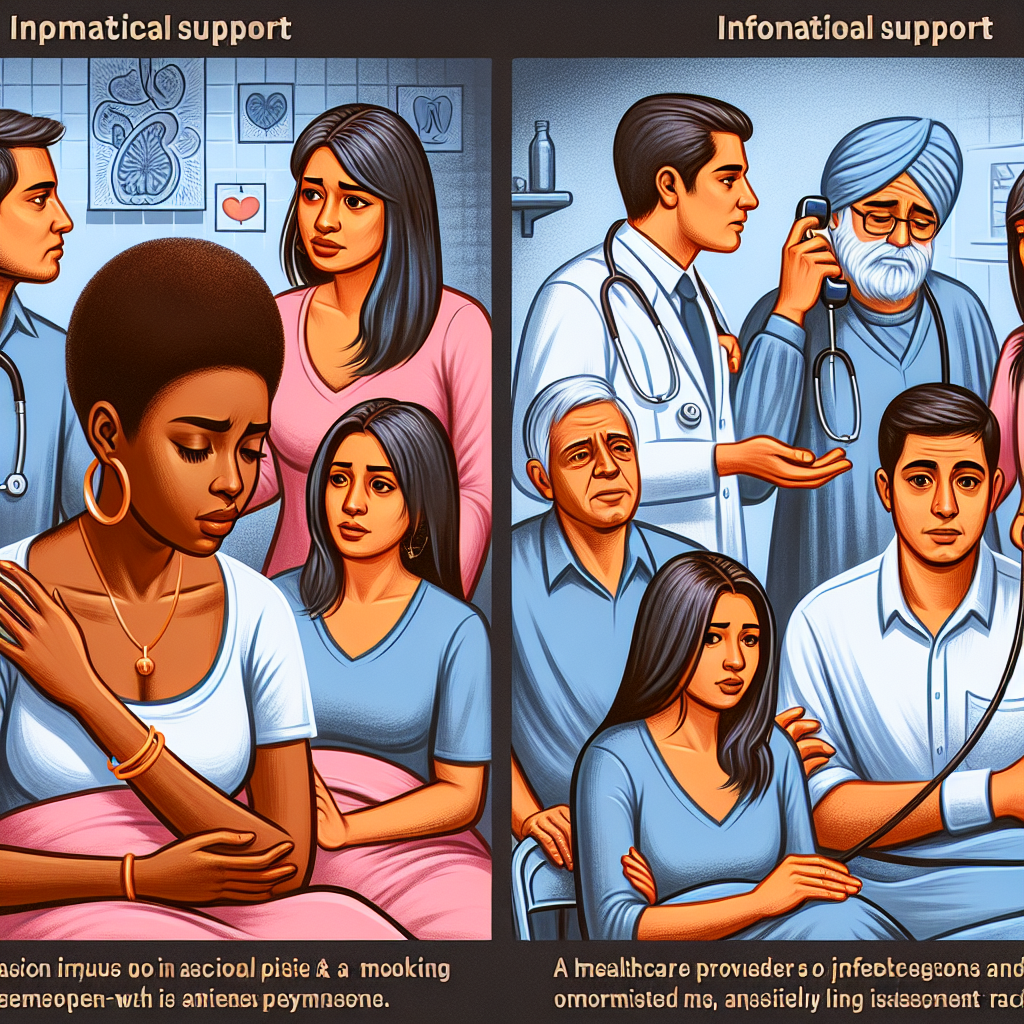
Living with Crohn’s disease creates unique challenges that shift our support needs in ways that healthy people often don’t understand. During active flares, emotional support becomes less about cheerful encouragement and more about having someone who can sit with us in the difficult moments without trying to fix everything. It’s about not having to put on a brave face when we’re struggling.
Informational support takes on new meaning too—those insights from others who’ve walked this path before us become invaluable guidance. And practical support, like help with groceries or household tasks when fatigue hits, can make the difference between managing and being overwhelmed.
During remission, our support needs evolve again. We need reassurance that our bodies can be trusted, gentle check-ins that don’t assume we’re always on the verge of another flare, and connections that help us stay informed about research and treatment advances. The fear of relapse never fully disappears, making ongoing connection and shared experiences crucial for maintaining mental health.
What This Means for the IBD Community
Research consistently shows that people with chronic illnesses who have strong social support networks experience significantly less anxiety and depression, better treatment adherence, and improved overall quality of life. For those of us with IBD, this isn’t just academic—it’s deeply personal and practical.
The isolation that often accompanies Crohn’s disease and ulcerative colitis can be devastating. Symptoms are unpredictable, treatments can be time-consuming and exhausting, and the invisible nature of our illness means others often don’t understand what we’re going through. This creates a perfect storm for social withdrawal, which research shows can actually worsen both physical symptoms and mental health outcomes.
Strong social connections provide several specific benefits for IBD patients. First, they offer emotional regulation during the stress of flares and treatment decisions. Having people who understand what we’re experiencing helps normalize our feelings and reduces the shame that often accompanies chronic illness. Second, informational support from peers can fill gaps that medical appointments sometimes miss—practical tips for managing symptoms, insights about treatment experiences, and navigation of healthcare systems.
Perhaps most importantly, social support helps maintain our sense of identity beyond our illness. When we’re connected to others who see us as whole people rather than collections of symptoms, we’re better able to maintain perspective during difficult periods and hope during uncertain times.
The challenge for many IBD patients is that our condition can make it harder to maintain traditional social connections. We might miss gatherings due to symptoms, have dietary restrictions that complicate social eating, or simply feel too exhausted to engage. This means we often need to be more intentional about building and maintaining our support networks.
Online communities have become incredibly valuable for IBD patients, offering 24/7 access to people who understand our experiences. These platforms allow us to connect during flares when leaving the house isn’t possible, share experiences anonymously when we’re not ready to discuss our condition with people in our immediate circles, and access a broader range of perspectives than might be available locally.
For caregivers and family members, understanding how to provide effective support can be challenging. The key is recognizing that support needs change based on disease activity and individual circumstances. During flares, practical help and emotional presence often matter more than advice. During remission, encouragement to engage in normal activities and gentle accountability for self-care can be most valuable.
Healthcare providers also play a crucial role in facilitating social support. Referring patients to support groups, connecting them with other patients when appropriate, and acknowledging the importance of mental health and social connection in overall treatment plans can significantly impact outcomes.
One area that deserves particular attention is the workplace. Many IBD patients struggle with disclosure decisions and worry about how their condition might affect professional relationships. Building supportive relationships with understanding colleagues and supervisors can reduce work-related stress, which often triggers symptom flares.
The timing of support is also crucial. Newly diagnosed patients need different types of connection than those who’ve been managing IBD for years. Parents of children with IBD need resources that address both their child’s needs and their own emotional processing. Young adults transitioning from pediatric to adult care need support networks that understand the unique challenges of managing a chronic illness while building independence.
Looking at broader trends in IBD care, there’s growing recognition that psychosocial factors significantly impact disease outcomes. This means that building strong support networks isn’t just about feeling better emotionally—it can actually influence our physical health and treatment success. Some IBD centers are beginning to integrate social workers, peer mentors, and mental health professionals into their care teams, recognizing that comprehensive treatment must address social and emotional needs alongside medical management.
Building Your Support Network
Creating an effective support network requires intentionality, especially when dealing with a condition that can be unpredictable and isolating. Start by identifying the different types of support you need: emotional (people who listen and validate your experience), informational (those who can share knowledge and resources), practical (help with daily tasks during difficult times), and social (connections that maintain your sense of normalcy and fun).
Consider questions you might discuss with your healthcare team: How can I communicate my support needs to family and friends? What resources are available in my community for IBD patients? How do I balance being open about my condition with maintaining privacy? When might professional counseling or therapy be beneficial?
Remember that asking for help is not a sign of weakness—it’s a crucial component of effective disease management. The people who care about you want to help, but they often don’t know how. Being specific about what you need and when you need it can strengthen your relationships rather than burden them.
The bottom line is that living well with Crohn’s disease or ulcerative colitis requires more than excellent medical care—it requires connection, understanding, and community. The research is clear that social support isn’t just nice to have; it’s a critical component of comprehensive IBD management. Whether that support comes from family, friends, online communities, or IBD-specific groups, investing in these connections is investing in your overall health and wellbeing. You don’t have to face this journey alone, and the effort you put into building and maintaining supportive relationships will pay dividends in every aspect of your life with IBD.
IBD Movement provides information for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.







