AI-Powered Hope: Personalized Nutrition for IBD Becomes Reality
If you live with IBD, you know the daily dance with food—carefully considering every meal, wondering if that supposedly “healthy” salad will trigger a flare, or if the comfort food that helped yesterday will betray you today. It’s exhausting to treat every bite like a gamble, especially when generic dietary advice feels like it was written for someone else’s body entirely.
But what if science could finally catch up to what we’ve always known—that IBD affects each of us differently, and our nutritional needs are just as unique as our symptoms?
Summary of University of Ottawa research
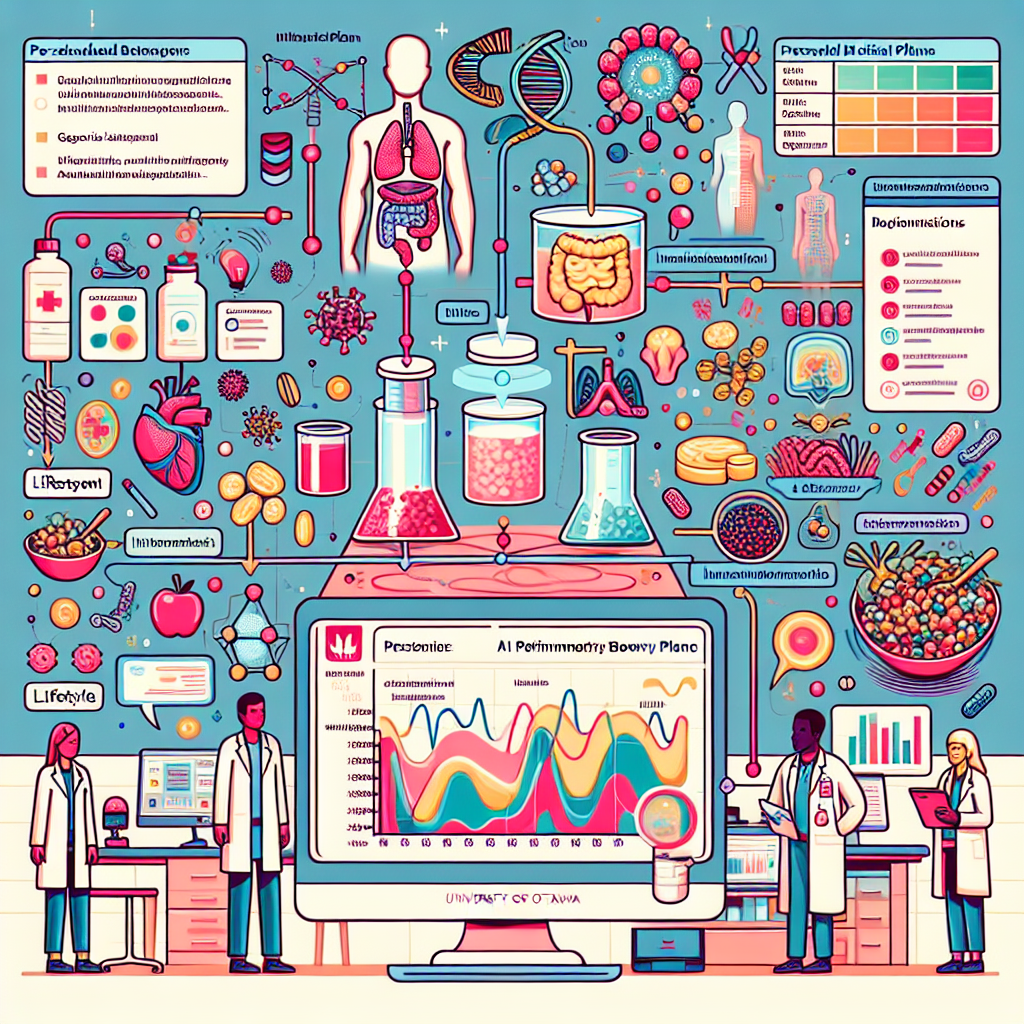
Researchers at the University of Ottawa have developed an innovative AI-powered tool designed specifically to create personalized nutrition plans for people with inflammatory bowel disease. Unlike generic diet apps or one-size-fits-all recommendations, this technology analyzes multiple individual factors including genetics, gut microbiome composition, lifestyle patterns, and personal health history to generate customized dietary guidance.
The tool addresses a fundamental challenge in IBD management: the wide variation in how different patients respond to foods and dietary interventions. While medication advances have improved IBD treatment, many patients continue to struggle with symptoms and flare-ups, making personalized nutrition support a critical need. This AI-driven approach aims to move beyond trial-and-error dietary management by providing evidence-based, individualized recommendations that can adapt as a person’s condition and needs change over time.
This post summarizes reporting from University of Ottawa research. Our analysis represents IBD Movement’s perspective and is intended to help patients understand how this news may affect them. Read the original article for complete details.
What This Means for the IBD Community
This development represents something many of us have been waiting for—validation that our individual experiences with food and IBD symptoms aren’t just in our heads, and that personalized care should extend beyond medication to include nutrition. For too long, we’ve been handed generic elimination diets or told to “eat more fiber” without consideration for our unique biology, symptom patterns, or life circumstances.
The potential impact on daily life could be transformative. Imagine having confidence in your meal planning because your dietary choices are backed by analysis of your specific genetic markers, gut bacteria profile, and symptom patterns. Instead of avoiding entire food groups out of fear, you might discover that certain foods you’ve been avoiding are actually beneficial for your particular IBD presentation, while others you thought were safe might be contributing to inflammation.
For caregivers and family members, this technology could provide much-needed clarity and reduce the frustration that comes with watching a loved one struggle to find foods that work. No more well-meaning advice about diets that worked for “someone they know” or confusion about conflicting dietary recommendations from different sources.
From a practical standpoint, this AI tool could significantly reduce the time and emotional energy currently spent on dietary trial and error. Many of us have spent months or even years trying different approaches—the specific carbohydrate diet, low-FODMAP, anti-inflammatory protocols—often with mixed or temporary results. A personalized approach could streamline this process and provide more consistent outcomes.
Several important questions emerge that you might want to discuss with your healthcare team: How would this technology integrate with your current treatment plan? Would insurance cover personalized nutrition analysis? How often would recommendations need to be updated as your condition changes? And perhaps most importantly, how do we balance evidence-based personalized recommendations with our own lived experience and food preferences?
This development also connects to broader trends we’re seeing in IBD research, particularly the growing recognition of the gut microbiome’s role in disease management and the move toward precision medicine approaches. We’re witnessing a shift from treating IBD as a single condition to understanding it as a spectrum of related disorders that require individualized strategies.
What excites me most about this research is that it validates something the IBD community has long understood: we are not broken versions of healthy people who just need to “eat better.” We have complex, individual biology that deserves sophisticated, personalized care. This technology suggests that the medical community is finally catching up to what we’ve been advocating for—treatment approaches that honor our individual experiences and needs.
However, it’s important to maintain realistic expectations. Even the most advanced AI tool will likely require human interpretation and adjustment. Your relationship with your gastroenterologist, registered dietitian, and other healthcare providers remains crucial. This technology should enhance, not replace, professional medical guidance and your own body awareness.
The research also highlights the importance of comprehensive data collection, which means patients who choose to use such tools in the future will need to be comfortable sharing detailed health information. For our community, which often deals with privacy concerns around IBD symptoms and bathroom habits, this raises important considerations about data security and patient control over personal health information.
Looking Forward: Hope with Realistic Expectations
While this AI-driven nutrition tool is still in development and not yet available to patients, it represents hope for a future where managing IBD through diet becomes less stressful and more effective. The fact that researchers are investing in IBD-specific nutrition technology shows that our unique needs are being recognized and addressed by the scientific community.
For now, this news reminds us that personalized nutrition for IBD is an active area of research with real potential. While we wait for these tools to become available, we can continue building relationships with healthcare providers who understand the complexity of IBD and nutrition, keeping detailed food and symptom journals, and advocating for individualized care approaches in our current treatment plans.
IBD Movement provides information for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.







