New Hope: Guselkumab Brings Targeted Relief to IBD Patients
There’s a moment that happens when you’ve been living with IBD for years—when you hear about yet another “breakthrough” treatment and feel that familiar mix of hope and hesitation. You want to believe that this time might be different, but you’ve been disappointed before. The medications that worked for others didn’t work for you, or the side effects were worse than the symptoms themselves. So when news breaks about a new therapy like guselkumab, it’s natural to approach it with cautious optimism.
But sometimes, that caution gives way to genuine excitement—especially when the science behind a new treatment represents a fundamental shift in how we understand and target IBD. That’s exactly what’s happening with guselkumab, a biologic therapy that’s been making waves in the IBD community for its precision approach to inflammation.
Summary of Pharmaceutical Journal
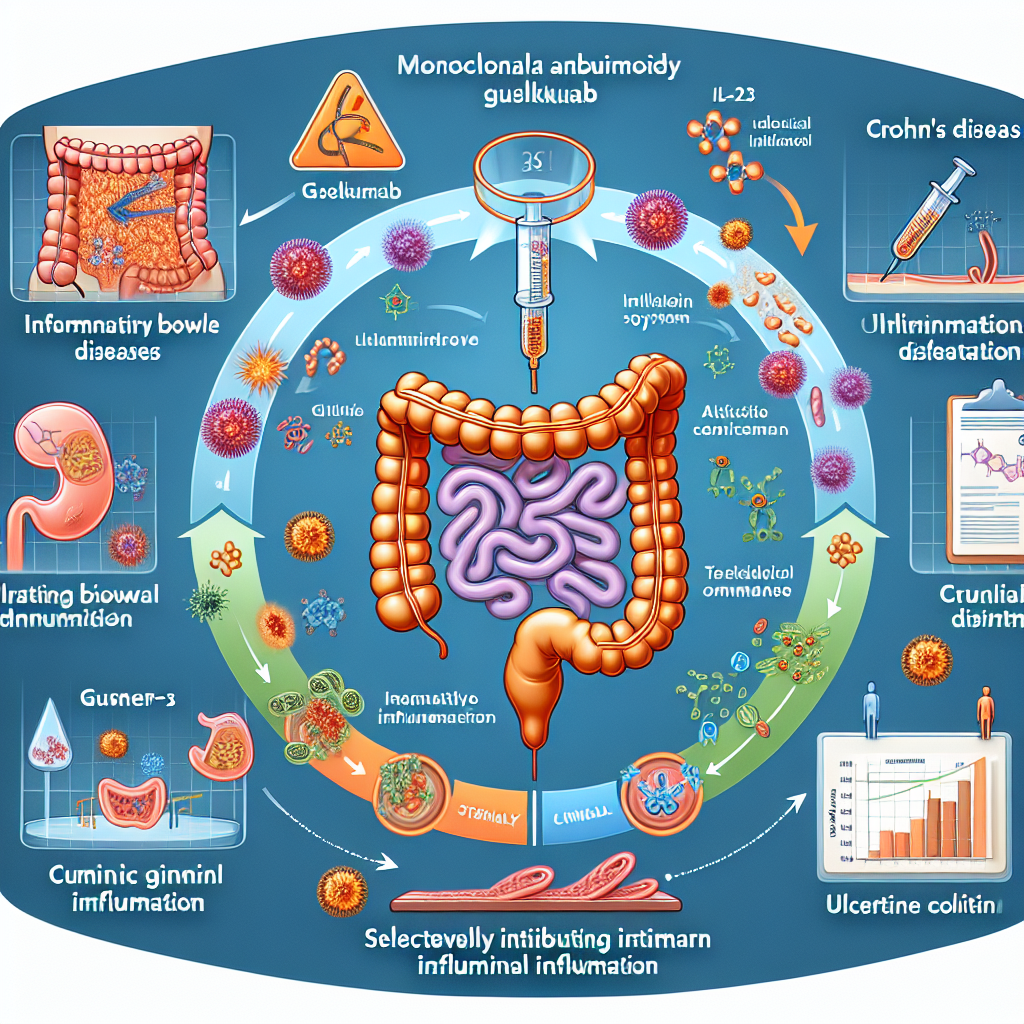
Guselkumab has recently received approval for treating moderate to severe Crohn’s disease and ulcerative colitis, marking a significant advancement in IBD care. This biologic therapy works by specifically targeting interleukin-23 (IL-23), a protein that plays a crucial role in driving intestinal inflammation. Clinical trials have shown impressive results, with over half of Crohn’s patients achieving remission at 12 weeks, and many patients experiencing symptom improvement as early as four weeks after starting treatment. The therapy has also demonstrated effectiveness in ulcerative colitis patients, with a favorable safety profile that gives both patients and doctors confidence in its long-term use.
This post summarizes reporting from Pharmaceutical Journal. Our analysis represents IBD Movement’s perspective and is intended to help patients understand how this news may affect them. Read the original article for complete details.
What This Means for the IBD Community
The approval of guselkumab represents more than just another treatment option—it signals a evolution in how we approach IBD therapy. For years, many of our treatments have taken a broad approach to inflammation, essentially using a sledgehammer when what we really needed was a scalpel. Guselkumab’s targeted approach to IL-23 represents that scalpel, offering precision that could mean fewer side effects and more effective symptom control.
For patients who have struggled with traditional therapies like mesalamine, corticosteroids, or even other biologics, guselkumab opens a new pathway. The IL-23 pathway is particularly significant because research has shown it to be a key driver of the chronic inflammation that characterizes both Crohn’s disease and ulcerative colitis. By blocking this specific protein, guselkumab addresses inflammation at its source rather than trying to manage its downstream effects.
What’s especially encouraging is the timeline for symptom improvement. Many IBD patients know the frustration of starting a new medication and waiting months to see if it will work. The fact that some patients in clinical trials experienced relief within four weeks is remarkable—it means less time spent in that anxious waiting period, wondering if this treatment will be “the one.”
The strong safety profile is equally important. IBD patients often find themselves weighing the benefits of symptom control against the risks of treatment side effects. When you’re already dealing with a chronic illness, the last thing you want is a treatment that creates new problems. The favorable safety data for guselkumab suggests that patients may be able to achieve better symptom control without significant additional health risks.
Questions to Consider for Your Healthcare Team
If you’re currently struggling with your IBD management, this development opens up important conversations with your gastroenterologist. Consider discussing:
- Whether your current treatment regimen is providing optimal symptom control and quality of life
- If you might be a candidate for guselkumab based on your specific disease characteristics and treatment history
- How this targeted approach might fit into your overall treatment strategy
- What the timeline might look like for accessing this therapy, including insurance considerations
- How guselkumab compares to other biologic options you may have tried or considered
It’s also worth discussing your treatment goals with your team. Are you looking for better symptom control, fewer side effects, or perhaps the ability to reduce dependence on corticosteroids? Understanding what success looks like for you personally can help guide treatment decisions.
The Bigger Picture in IBD Research
Guselkumab’s success reflects a broader trend in IBD research toward precision medicine. We’re moving away from one-size-fits-all approaches and toward treatments that target specific pathways involved in disease progression. This represents years of research into the underlying mechanisms of IBD paying off in real-world therapeutic advances.
The IL-23 pathway that guselkumab targets is also being investigated in other inflammatory conditions, which suggests that the insights gained from IBD research may have broader applications. This interconnected approach to understanding inflammation could lead to even more targeted therapies in the future.
For the IBD community, this progress is particularly meaningful because it validates what patients have long known—that IBD is a complex disease requiring sophisticated treatment approaches. The fact that researchers and pharmaceutical companies are investing in these targeted therapies shows a commitment to improving outcomes for people living with chronic inflammatory conditions.
Managing Expectations and Hope
While the clinical trial results for guselkumab are encouraging, it’s important to remember that every person’s IBD journey is unique. What works remarkably well for one patient may not be as effective for another. The key is having options—and guselkumab represents one more valuable tool in the IBD treatment toolkit.
For patients who have experienced treatment fatigue or who feel like they’ve exhausted their options, knowing that innovative therapies like guselkumab are becoming available can provide a renewed sense of hope. The field of IBD treatment continues to evolve rapidly, with new understanding of disease mechanisms leading to more targeted and effective therapies.
It’s also worth noting that optimal IBD management often involves more than just medication. Stress management, nutrition, sleep, and other lifestyle factors continue to play important roles in overall well-being. Guselkumab and other advanced therapies work best as part of a comprehensive approach to IBD care.
The approval of guselkumab sends a clear message to the IBD community: researchers and clinicians are listening to patients’ needs and working to develop better solutions. This isn’t just about managing symptoms—it’s about restoring quality of life, enabling people to pursue their goals, and reducing the daily burden that IBD can place on individuals and families.
For caregivers and family members, this development is equally significant. Watching a loved one struggle with IBD can feel helpless at times. Knowing that new, more effective treatments are becoming available provides hope not just for patients, but for everyone who supports them on their health journey.
The journey with IBD is rarely straightforward, and new treatments like guselkumab don’t promise perfection. What they do offer is progress—measurable, meaningful improvements in how we can control inflammation and help people reclaim their lives from chronic illness. In a condition where small improvements can make enormous differences in daily quality of life, that progress is everything.
Ultimately, guselkumab represents hope backed by solid science. It’s a reminder that the IBD community doesn’t have to accept the status quo, and that continued research and advocacy can lead to real improvements in care. For anyone currently struggling with inadequate symptom control or treatment side effects, this development opens new possibilities worth exploring with your healthcare team.
IBD Movement provides information for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.







