Crohn’s Stricture Management: When Your Intestines Start Narrowing
Introduction
If you’ve been living with Crohn’s disease, the word “stricture” might send a chill down your spine—and for good reason. Strictures represent one of the most concerning complications of Crohn’s disease, affecting up to 30% of people with the condition over their lifetime. When chronic inflammation causes your intestinal walls to thicken and narrow, it creates a bottleneck that can significantly impact your quality of life and digestive function.
This question about stricture management comes up frequently in gastroenterology offices, online support groups, and among newly diagnosed patients who are learning about potential complications. Whether you’re experiencing symptoms that suggest a stricture, have recently been diagnosed with one, or are simply preparing for what might lie ahead, understanding how to manage intestinal narrowing is crucial for maintaining your health and peace of mind.
The good news? While strictures are serious, they’re manageable with the right approach, timing, and medical team. Let’s explore everything you need to know about navigating this challenging aspect of Crohn’s disease.
The Short Answer
Crohn’s stricture management involves a multi-layered approach that includes dietary modifications, medication optimization, and careful monitoring, with surgical intervention reserved for severe cases. The key is early detection and proactive management—catching strictures before they become completely obstructive allows for more treatment options and better outcomes. Most people with strictures can maintain good quality of life through strategic dietary changes and appropriate medical care.
The Complete Answer
Managing Crohn’s strictures requires understanding that not all strictures are created equal. Some are inflammatory (caused by active swelling), others are fibrotic (caused by scar tissue), and many are a combination of both. This distinction matters enormously because it determines your treatment approach.
Understanding Stricture Development
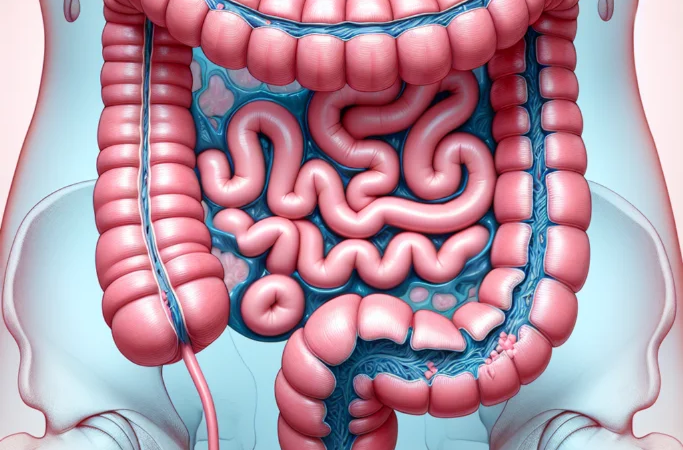
Strictures develop when repeated cycles of inflammation and healing create scar tissue that gradually narrows your intestinal passage. The small intestine is most commonly affected, particularly the terminal ileum where the small and large intestines meet. This narrowing can range from mild (causing occasional symptoms) to severe (creating complete blockages).
The progression isn’t always predictable. Some people develop strictures within months of diagnosis, while others live with Crohn’s for decades without significant narrowing. Factors that increase stricture risk include:
- Penetrating (fistulizing) Crohn’s disease behavior
- Small bowel involvement
- Smoking history
- Inadequate inflammation control over time
- Previous intestinal surgery
The Management Spectrum
Conservative Management forms the foundation of stricture care. This involves optimizing your anti-inflammatory medications to reduce ongoing inflammation that contributes to stricture formation. Your gastroenterologist might adjust your current therapy or introduce new medications like biologics if you’re not already on them.
Dietary modifications play a crucial role in day-to-day management. The goal is reducing the mechanical stress on narrowed areas while maintaining proper nutrition. This typically means:
- Adopting a low-residue diet during symptomatic periods
- Chewing food thoroughly and eating smaller, more frequent meals
- Avoiding high-fiber foods, nuts, seeds, and tough meats during flares
- Staying well-hydrated to help food move through narrowed areas
Endoscopic intervention has emerged as a valuable middle ground between medication and surgery. Balloon dilation, performed during colonoscopy, can stretch narrowed areas and provide symptom relief. This procedure is most effective for short, inflammatory strictures and can often be repeated if needed.
Surgical resection remains the definitive treatment for severe, symptomatic strictures that don’t respond to other measures. Modern surgical techniques, including laparoscopic approaches, have made these procedures less invasive with faster recovery times.
Timing Is Everything
The most critical aspect of stricture management is knowing when to escalate treatment. Waiting too long can lead to emergency situations, while acting too quickly might mean unnecessary procedures. Your healthcare team will monitor several factors:
- Frequency and severity of obstructive symptoms
- Nutritional status and weight maintenance
- Imaging findings showing progression
- Response to current medical therapy
- Impact on quality of life
What Patients Should Know
Recognizing warning signs is your first line of defense. Cramping abdominal pain, especially after eating, bloating, nausea, and changes in bowel habits can all signal stricture development or worsening. Don’t dismiss these symptoms as “just part of having Crohn’s”—they warrant medical evaluation.
Questions to ask your gastroenterologist about stricture management include:
- “What type of stricture do I have—inflammatory, fibrotic, or mixed?”
- “How severe is the narrowing, and has it changed since my last imaging?”
- “Am I a candidate for balloon dilation?”
- “What dietary changes should I make right now?”
- “At what point would you recommend surgery?”
- “How often should we monitor this with imaging?”
Red flags requiring immediate medical attention include:
- Severe, persistent abdominal pain
- Inability to keep food or liquids down
- No bowel movements or gas for more than 24 hours
- Significant abdominal distension
- Fever combined with obstructive symptoms
These symptoms could indicate a complete bowel obstruction, which is a medical emergency requiring immediate hospital care.
Nutritional monitoring becomes especially important with strictures. Work with a dietitian familiar with IBD to ensure you’re meeting your nutritional needs despite dietary restrictions. Regular blood work to check for deficiencies in vitamins B12, D, iron, and other nutrients is essential.
Related Questions
How can I tell if my stricture is getting worse? Progressive worsening typically involves increasing frequency of symptoms, longer duration of pain after eating, and needing to restrict your diet further. New or worsening nausea and vomiting are particularly concerning signs.
Can strictures heal or reverse on their own? Inflammatory strictures can improve significantly with proper medical treatment, but fibrotic strictures (made of scar tissue) generally don’t reverse without intervention. This is why early, aggressive treatment of inflammation is so important.
What’s the success rate of balloon dilation? Studies show that balloon dilation provides symptom relief in 70-80% of appropriate candidates, with many people remaining symptom-free for years. However, the procedure may need to be repeated, and not all strictures are suitable for this approach.
If I need surgery, will my Crohn’s come back? Surgery removes the diseased segment, but Crohn’s can recur in other areas. However, post-surgical medication protocols have significantly improved long-term outcomes, with many people maintaining remission for years after surgery.
The Bottom Line
Crohn’s stricture management is about finding the right balance between conservative care and more aggressive interventions, tailored to your specific situation. The key is developing a strong partnership with your gastroenterologist, staying vigilant about symptoms, and being proactive rather than reactive in your approach.
Remember that having a stricture doesn’t mean your life is over or that surgery is inevitable. Many people with strictures live full, active lives through careful management and lifestyle modifications. The medical field continues to develop new approaches, from improved medications to less invasive procedures.
Your next steps should include discussing your current symptoms honestly with your healthcare team, ensuring your current medications are optimally controlling inflammation, and developing an action plan for managing symptoms at home. Don’t hesitate to seek a second opinion if you’re unsure about treatment recommendations—stricture management often benefits from specialized expertise.
Most importantly, stay connected with your IBD community and healthcare team. Strictures can feel isolating and scary, but you’re not alone in this journey. With proper management, most people with Crohn’s strictures continue to live meaningful, fulfilling lives.







