Exercise with Crohn’s: Finding Your Path to Gentle Movement
If you’re living with Crohn’s disease, the word “exercise” might make you feel overwhelmed before you even start. Between managing symptoms, fatigue, and the unpredictability of flares, adding another “should” to your list can feel impossible. But here’s what I’ve learned from countless conversations with our IBD community: movement doesn’t have to look like what everyone else is doing—it just has to work for you.
The truth is, many of us have complicated relationships with exercise after our diagnosis. Maybe you were active before Crohn’s entered your life, or perhaps you’ve always felt intimidated by fitness culture. Either way, finding your path back to (or toward) movement when you’re managing a chronic condition requires a completely different mindset—one that prioritizes self-compassion over performance.
Summary of HealthCentral
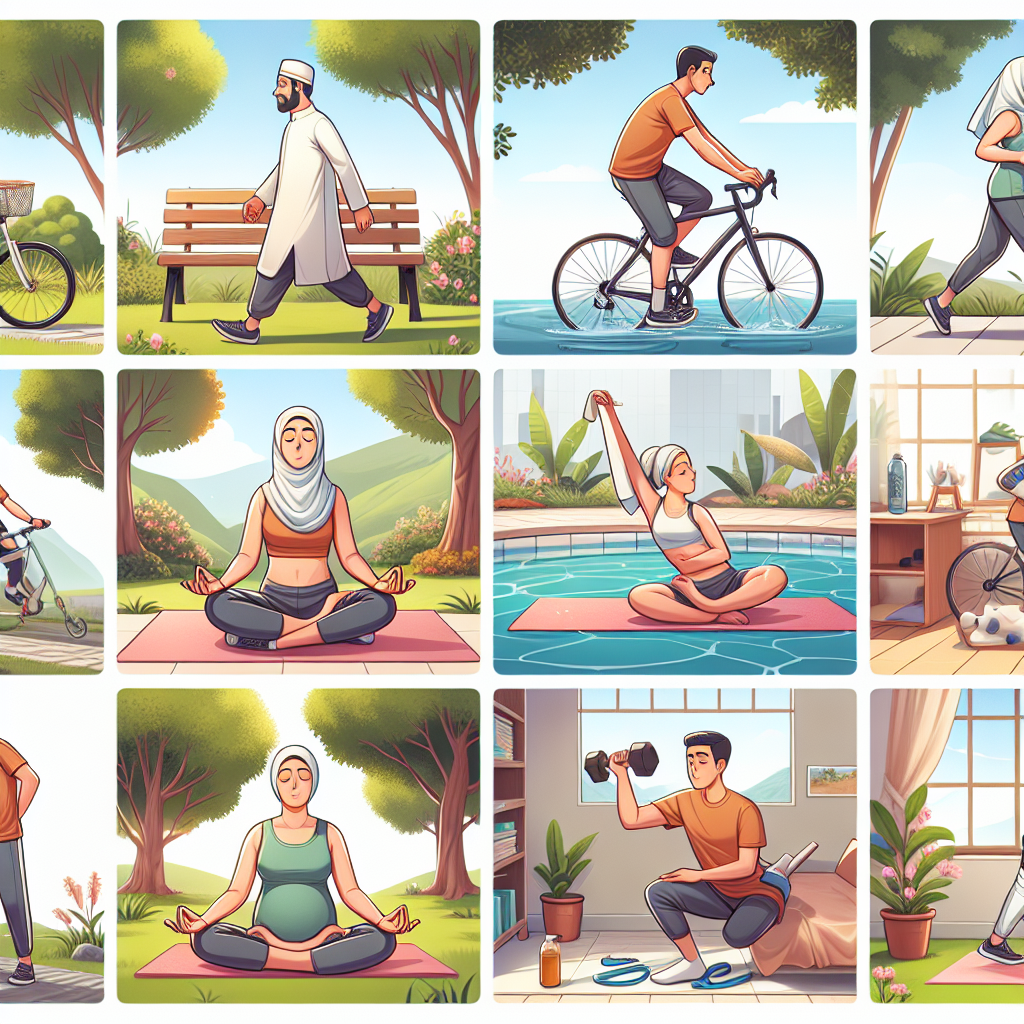
HealthCentral explores how exercise can be a powerful tool for managing Crohn’s disease, both physically and emotionally. The article emphasizes that movement doesn’t need to be intense or demanding—gentle activities like walking, yoga, or light cycling can provide significant benefits. Research shows that consistent, low-impact exercise can help reduce stress and anxiety, which are common triggers for Crohn’s flares.
The key message is starting small and choosing activities that feel supportive rather than punishing. The article suggests that even light gardening or stretching can boost energy levels without causing exhaustion. It stresses the importance of listening to your body and resting when needed, framing rest as part of the healing process rather than a failure. The overall approach encourages patience and celebrates small victories, recognizing that exercise success looks different for everyone living with Crohn’s.
This post summarizes reporting from HealthCentral. Our analysis represents IBD Movement’s perspective and is intended to help patients understand how this news may affect them. Read the original article for complete details.
What This Means for the IBD Community
This perspective on exercise represents a fundamental shift that our community desperately needs. For too long, we’ve been told to “push through” or “stay positive,” as if willpower alone could overcome the physical realities of living with Crohn’s. What HealthCentral gets right is acknowledging that exercise with IBD requires a completely different framework—one built on flexibility, self-awareness, and realistic expectations.
In my experience working with IBD patients, I’ve noticed that those who successfully incorporate movement into their lives share one common trait: they’ve learned to separate exercise from diet culture and fitness industry messaging. They don’t exercise to “earn” their meals or to achieve a certain body type. Instead, they move because it helps them feel more like themselves, reduces their anxiety, and gives them a sense of agency over their health.
The stress-reduction benefits mentioned in the article are particularly crucial for our community. We know that psychological stress can trigger flares, create a vicious cycle where anxiety about symptoms actually worsens symptoms. When you find movement that genuinely reduces your stress levels—whether that’s a gentle walk in nature, restorative yoga, or dancing in your living room—you’re not just improving your fitness. You’re potentially reducing your flare risk and improving your overall quality of life.
Here’s what I think many people don’t realize: exercise with Crohn’s often looks nothing like the Instagram fitness posts or the recommendations you’ll find in general health articles. Your “workout” might be:
- A 10-minute walk on days when you’re feeling good
- Gentle stretching in bed on mornings when getting up feels impossible
- Swimming laps when joint pain makes land-based exercise uncomfortable
- Yoga poses modified for abdominal tenderness
- Gardening that gets you moving without the pressure of a structured routine
The beautiful thing about this approach is that it honors where you are right now, not where you think you should be. It also acknowledges that your exercise capacity will fluctuate—and that’s not a personal failing, it’s the reality of living with a chronic condition.
From a practical standpoint, this means having multiple “movement options” ready for different symptom levels. On high-energy days, you might feel up for a longer walk or bike ride. On moderate days, maybe it’s gentle yoga or swimming. On low-energy days, perhaps it’s just stretching or deep breathing exercises. The key is having a toolkit rather than a rigid routine.
I also want to address something the article touches on but that deserves more emphasis: the psychological benefits of movement for IBD patients extend far beyond stress reduction. Exercise can help you reconnect with your body in a positive way. When you’re managing a chronic illness, it’s easy to view your body as unreliable or even as an adversary. Gentle, consistent movement can help rebuild trust and appreciation for what your body can do, rather than focusing solely on what it can’t.
For caregivers and family members reading this, understanding this perspective is crucial. Your loved one with Crohn’s isn’t being “lazy” if they can’t commit to regular gym sessions or if they need to modify their activity level frequently. Supporting their movement goals means celebrating the small victories, understanding that rest days are part of the plan, and helping them find activities that bring joy rather than stress.
Questions you might want to discuss with your healthcare team include:
- Are there specific types of exercise that might be better or worse for my particular Crohn’s presentation?
- How can I tell the difference between normal exercise fatigue and IBD-related fatigue?
- Should I modify my exercise routine during a flare, and if so, how?
- Are there any warning signs that suggest I should stop exercising and contact you?
- How might exercise interact with my current medications?
Building Your Personal Movement Practice
What I love about the approach outlined in the HealthCentral piece is that it encourages experimentation and personalization. There’s no one-size-fits-all exercise prescription for IBD patients because our symptoms, energy levels, and preferences are all different. The goal is to find what works for your body, your schedule, and your current health status.
One strategy that many IBD patients find helpful is what I call “movement stacking”—pairing gentle exercise with activities you already do. This might mean doing calf raises while brushing your teeth, taking phone calls while walking, or doing gentle stretches while watching TV. This approach removes the barrier of finding separate time for exercise and makes movement feel more integrated into daily life.
It’s also worth noting that the “gentle” approach doesn’t mean “ineffective.” Research consistently shows that moderate exercise provides significant health benefits, including improved mood, better sleep, enhanced immune function, and reduced inflammation. For IBD patients, these benefits can be particularly valuable in managing overall health and potentially reducing the frequency or severity of symptoms.
The bottom line is this: you don’t need to become a fitness enthusiast or follow anyone else’s definition of an active lifestyle. You just need to find ways of moving that make you feel better, both physically and emotionally. Some days that might be a vigorous walk, other days it might be gentle stretching in bed. Both count, both matter, and both deserve to be celebrated.
Remember that building a sustainable movement practice with IBD is a marathon, not a sprint. Be patient with yourself as you figure out what works, and don’t hesitate to adjust your approach as your symptoms and energy levels change. The fact that you’re even considering how to incorporate more movement into your life shows tremendous self-care and hope for your future—and that’s something to be proud of, regardless of how many steps you take or how many yoga poses you can do.
IBD Movement provides information for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.







