New Microgel Technology Could Target Harmful Bacteria in IBD
If you’re living with IBD, you know that feeling when your gut seems to have a mind of its own. One day you’re managing well, the next you’re dealing with inflammation that seems to come from nowhere. For many of us in the Crohn’s and colitis community, the search for solutions that work with our bodies—not against them—feels endless. What if I told you that researchers are developing a completely new approach that could intercept harmful bacteria before they even trigger inflammation?
This isn’t another medication to add to your routine. Instead, scientists are creating microscopic “decoys” that could outsmart the bacteria causing problems in our intestines. It’s the kind of innovation that makes you pause and think: maybe we’re finally getting closer to treatments that address IBD at its source.
Summary of https://bioengineer.org/microgels-harness-fimh-to-capture-aiec-bacteria/
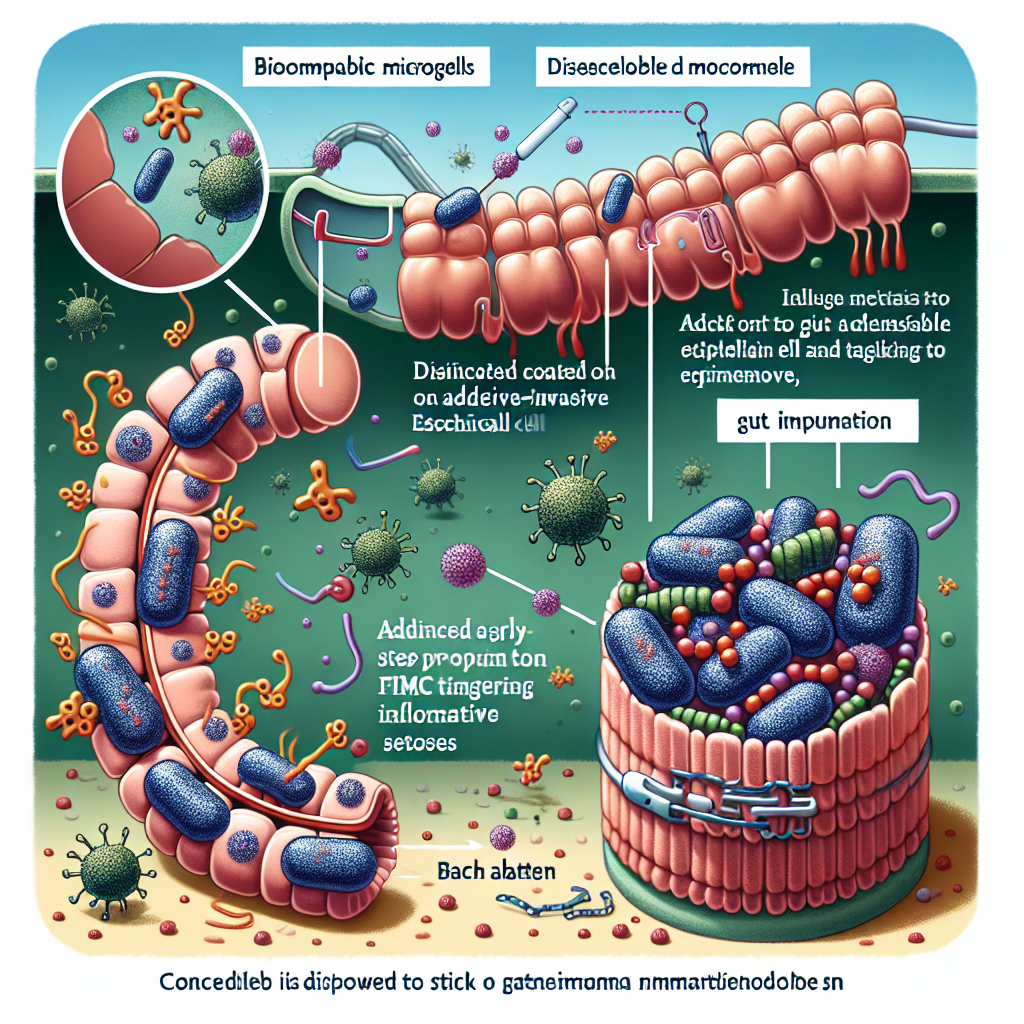
Researchers have developed tiny gel particles called microgels that are coated with a sugar molecule called mannose. These microscopic spheres work like biological mousetraps for a specific type of harmful bacteria called AIEC (adherent-invasive E. coli) that’s commonly found in people with Crohn’s disease.
Here’s how it works: AIEC bacteria have finger-like projections called fimbriae that help them stick to the intestinal wall. These bacteria use a protein called FimH to grab onto mannose sugars naturally present on our intestinal cells. Once attached, they can invade the tissue and trigger the inflammatory response we know all too well.
The mannose-coated microgels act as decoys, attracting the bacteria away from intestinal cells. Instead of attaching to and invading the gut wall, the bacteria bind to these harmless gel particles and can then be naturally eliminated from the body. The approach specifically targets the mechanism these bacteria use to cause damage, potentially stopping inflammation before it starts.
This post summarizes reporting from https://bioengineer.org/microgels-harness-fimh-to-capture-aiec-bacteria/. Our analysis represents IBD Movement’s perspective and is intended to help patients understand how this news may affect them. Read the original article for complete details.
What This Means for the IBD Community
As someone who follows IBD research closely, I find this microgel approach particularly exciting because it represents a fundamental shift in how we might treat inflammatory bowel disease. Instead of suppressing our immune system or broadly targeting inflammation after it’s already started, this technology aims to prevent the trigger in the first place.
For those of us living with Crohn’s disease, the connection to AIEC bacteria is especially relevant. Studies have shown that up to 60% of people with Crohn’s have higher levels of AIEC in their intestines compared to healthy individuals. These bacteria aren’t just innocent bystanders—they actively contribute to the chronic inflammation that makes daily life so challenging.
What makes this approach different from current treatments is its precision. Think about it this way: most IBD medications work like using a fire hose to put out a candle. They’re effective, but they can also affect healthy parts of your immune system and gut bacteria. This microgel technology is more like using tweezers to remove the specific match that’s lighting the fire.
The implications for quality of life could be significant. Many of us have experienced the frustration of treatments that help with symptoms but don’t address underlying causes. We’ve dealt with the side effects of immunosuppressants, the unpredictability of biologics losing effectiveness, and the constant worry about long-term consequences of our medications. A targeted approach like this could potentially offer symptom relief without some of these trade-offs.
From a practical standpoint, if this technology moves forward, it could change how we think about IBD management. Instead of waiting for flares to treat them, we might be able to prevent them by regularly clearing harmful bacteria from our systems. This preventive approach aligns with what many of us already try to do through diet, probiotics, and lifestyle changes—but with much more precision and scientific backing.
However, it’s important to manage expectations. This research is still in early stages, and we don’t yet know how effective it would be in real-world conditions. Our digestive systems are incredibly complex, and what works in laboratory settings doesn’t always translate directly to clinical success. Additionally, IBD involves multiple factors beyond AIEC bacteria, so this approach might work best as part of a comprehensive treatment strategy rather than a standalone solution.
For patients and caregivers, this research raises several important questions worth discussing with your healthcare team:
- Could testing for AIEC bacteria levels help personalize your treatment approach?
- How might targeted bacterial therapies fit into your current treatment regimen?
- What other emerging therapies focus on addressing root causes rather than just managing symptoms?
- How do you balance hope for new treatments with realistic expectations about timelines?
This microgel development also fits into a broader trend in IBD research toward personalized, mechanism-based treatments. We’re seeing similar innovations in areas like fecal microbiota transplantation, engineered probiotics, and targeted immune therapies. The common thread is a move away from one-size-fits-all approaches toward treatments tailored to individual disease mechanisms.
What gives me particular hope about this research is that it emerges from a deep understanding of IBD pathophysiology. The researchers didn’t just create a new drug and hope it would work—they identified a specific problem (AIEC adhesion and invasion) and engineered a targeted solution. This kind of precision medicine approach represents the future of IBD treatment.
For those dealing with treatment-resistant Crohn’s disease or looking for alternatives to current therapies, research like this provides reason for cautious optimism. While we wait for clinical trials and regulatory approval processes, it’s encouraging to know that scientists are thinking creatively about IBD solutions and that the field continues to advance toward more targeted, effective treatments.
The Bottom Line
This microgel technology represents the kind of innovative thinking our community needs—treatments that work with our bodies’ natural processes rather than against them. While it’s still early in development, the approach of using biological decoys to prevent bacterial adhesion and inflammation offers a glimpse into a future where IBD treatment might be more targeted and potentially more effective.
As we’ve learned from other breakthrough treatments, the path from laboratory discovery to patient access can be long and uncertain. But research like this reminds us that scientists are continuously working to understand and address the root causes of our condition, not just its symptoms. That dedication to finding better solutions gives me hope that the future of IBD care will be brighter than what we experience today.
IBD Movement provides information for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.







