The Stress-IBD Connection: What Every Patient Should Know
If you’re living with IBD, you’ve probably been there: doubled over with pain, wondering if the mounting stress in your life is making everything worse. Maybe you’ve even questioned whether stress caused your Crohn’s disease or ulcerative colitis in the first place. It’s a natural assumption—after all, we can physically feel our emotions in our gut.
But here’s the thing: the relationship between stress and IBD is far more complex than many of us realize. While stress doesn’t actually cause IBD, it plays a significant role in our day-to-day experience with the condition. Understanding this distinction isn’t just academic—it’s crucial for how we manage our health and seek appropriate care.
Summary of Is Your Inflammatory Bowel Disease Really Caused By Stress? Expert Tells
Recent expert insights from Dr. Amar J Inder Singh, Senior Consultant in Gastroenterology, help clarify this often-misunderstood relationship. According to the article, while stress isn’t a direct cause of IBD, it can significantly worsen existing symptoms and trigger flare-ups in those already living with the condition.
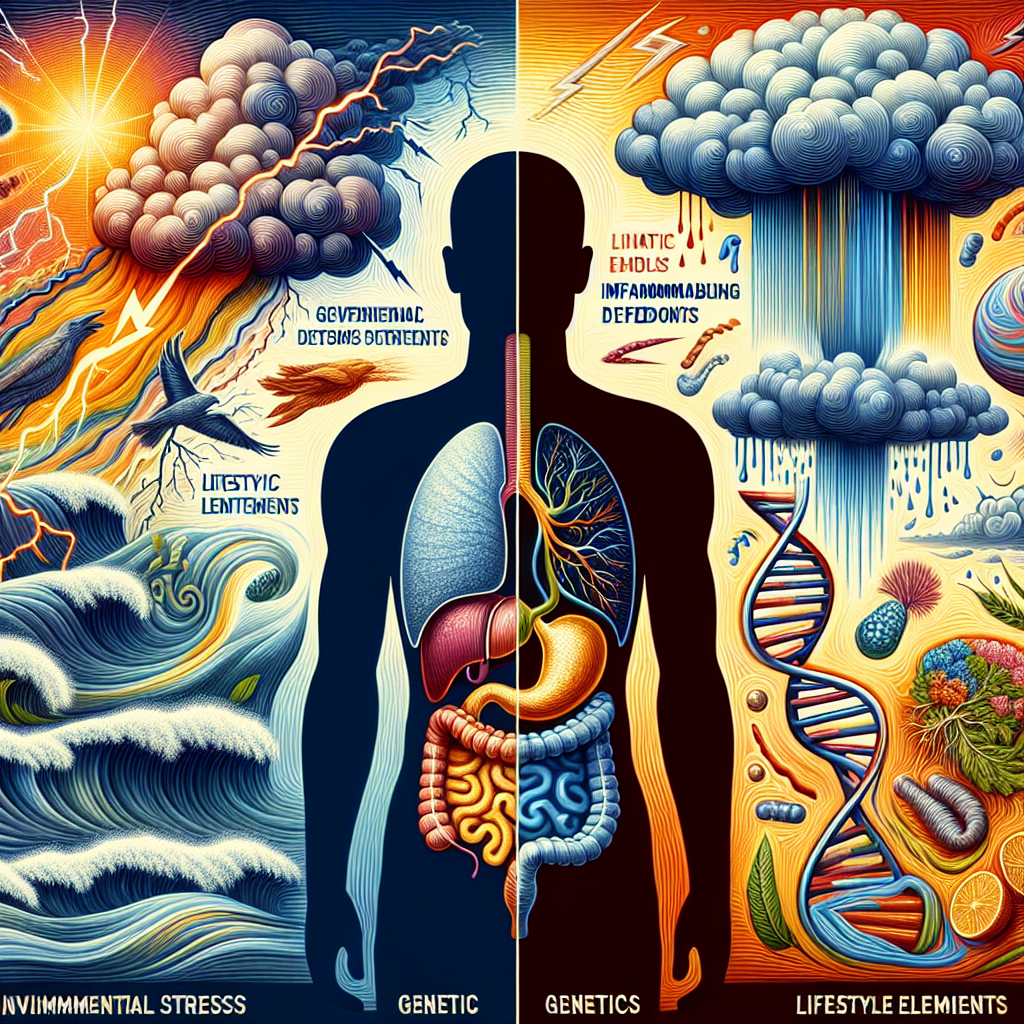
IBD—which includes Crohn’s disease and ulcerative colitis—affects millions worldwide through chronic inflammation of the digestive tract. The true causes remain somewhat mysterious, but research points to a combination of genetic predisposition, immune system dysfunction, environmental triggers, and lifestyle factors.
Dr. Singh explains that stress can negatively impact digestive function and immune response, making symptoms worse for those already diagnosed. However, the root causes typically involve genetic factors, immune dysregulation, and external triggers like infections or certain medications—not stress alone.
The expert emphasizes the importance of not dismissing persistent digestive symptoms as “just stress.” While emotional stress can manifest as abdominal pain or irregular bowel movements, chronic symptoms like persistent diarrhea, blood in stools, unintended weight loss, and fatigue require professional medical evaluation.
This post summarizes reporting from Is Your Inflammatory Bowel Disease Really Caused By Stress? Expert Tells. Our analysis represents IBD Movement’s perspective and is intended to help patients understand how this news may affect them. Read the original article for complete details.
What This Means for the IBD Community
This clarification about stress and IBD carries profound implications for how we understand and manage our condition. First and foremost, it validates something many of us have experienced: stress absolutely can make our symptoms worse, even if it didn’t cause our IBD in the first place.
For those still seeking a diagnosis, this information is particularly valuable. How many of us have been told our symptoms are “just stress” or “all in our head” before receiving proper medical evaluation? This expert perspective reinforces why we must advocate for thorough testing when experiencing persistent digestive symptoms, regardless of our stress levels.
The mind-gut connection is real and powerful. When we’re stressed, our bodies produce cortisol and other stress hormones that can increase inflammation, alter gut bacteria, and affect digestive function. For those of us with IBD, this means stress management isn’t just about feeling better emotionally—it’s a crucial component of our overall treatment strategy.
This understanding also helps explain why some of us notice patterns in our flare-ups. Major life events, work pressure, relationship stress, or even positive stressors like weddings or job promotions might correlate with symptom increases. Recognizing these patterns can help us prepare and implement coping strategies proactively.
However, it’s equally important that this knowledge doesn’t lead to self-blame. If you’re experiencing a flare-up during a stressful period, it doesn’t mean you’ve “caused” your symptoms or that you’re not managing stress well enough. IBD is a complex medical condition with multiple contributing factors, and stress is just one piece of a much larger puzzle.
For caregivers and family members, this information is also crucial. Understanding that stress can worsen symptoms—but doesn’t cause the underlying disease—can help loved ones provide appropriate support without inadvertently suggesting that stress management alone will “cure” the condition.
From a practical standpoint, this research supports the growing emphasis on integrated IBD care that addresses both physical and mental health. Many IBD centers now include mental health professionals, nutritionists, and stress management resources as part of comprehensive treatment teams.
Consider discussing these topics with your gastroenterologist at your next appointment:
- How stress might be affecting your specific symptoms
- Whether stress management techniques could complement your current treatment plan
- What warning signs to watch for that might indicate stress-related symptom worsening
- Whether a referral to a mental health professional experienced with chronic illness would be beneficial
This expert perspective also highlights why symptom tracking can be so valuable. Recording not just physical symptoms but also stress levels, major life events, and emotional well-being can help identify patterns and triggers that might otherwise go unnoticed.
The broader implications extend to IBD research as well. As we better understand the complex interactions between stress, inflammation, and immune function, new therapeutic approaches may emerge. Some promising areas include targeted stress reduction interventions, mindfulness-based therapies specifically designed for IBD patients, and medications that address both physical inflammation and stress response.
For the IBD community, this research reinforces that taking care of our mental health isn’t a luxury—it’s a medical necessity. Whether through therapy, meditation, exercise, hobby engagement, or other stress management techniques, prioritizing emotional well-being can be as important as taking our medications consistently.
Moving Forward with This Knowledge
Understanding the true relationship between stress and IBD empowers us to take a more comprehensive approach to our health. It validates the very real impact stress has on our symptoms while reinforcing that IBD is a legitimate medical condition requiring professional treatment.
This knowledge encourages us to be proactive about stress management without falling into the trap of believing we can control our IBD through stress reduction alone. It’s about finding balance—acknowledging stress as one important factor among many, while continuing to work closely with our medical teams on evidence-based treatments.
IBD Movement provides information for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.







