Hidden Gut Engine Discovery Offers New Hope for Crohn’s Patients
Have you ever wondered what’s really happening inside your gut when Crohn’s flares strike? That churning, unpredictable feeling that seems to have a mind of its own? You’re not alone in feeling like your digestive system is running on some mysterious engine that you can’t control or understand.
For those of us living with Crohn’s disease, our bodies often feel like they’re working against us. But what if I told you that scientists have just discovered a hidden mechanism in our guts that could explain why things go wrong—and more importantly, how we might fix them?
Summary of Scientists uncover the gut’s hidden hydrogen engine and how it falters in Crohn’s disease
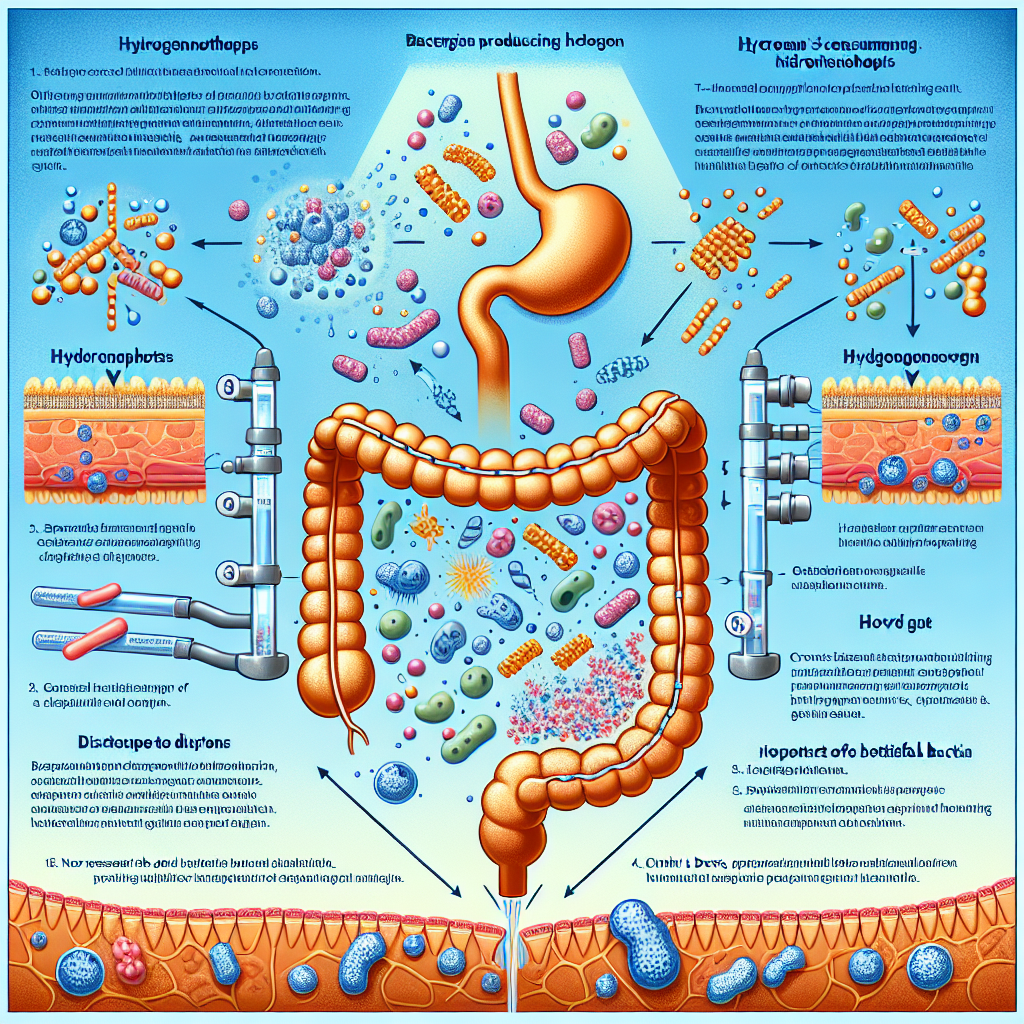
Researchers have identified what they’re calling a “hidden hydrogen engine” in our digestive systems. Here’s how it works: when we eat, certain gut bacteria naturally produce hydrogen gas as they break down our food. In a healthy gut, specialized bacteria called hydrogenotrophs quickly remove this hydrogen, keeping everything balanced.
Think of it like a well-oiled factory assembly line. Food comes in, gets processed, hydrogen gets produced as a byproduct, and then gets cleaned up by these helper bacteria. Everyone has a job, and the system runs smoothly.
But in people with Crohn’s disease, this system breaks down. The study found that Crohn’s patients have fewer of these hydrogen-removing bacteria. When hydrogen starts building up because there aren’t enough “cleanup crew” bacteria, it disrupts the entire gut ecosystem. This imbalance may contribute to the inflammation and digestive problems that make Crohn’s so challenging to live with.
The researchers used advanced genetic testing to analyze tissue and stool samples from both healthy people and those with Crohn’s. They mapped out the bacterial communities and measured how well they processed hydrogen, revealing this crucial difference in the “hydrogen engine’s” function.
This post summarizes reporting from Scientists uncover the gut’s hidden hydrogen engine and how it falters in Crohn’s disease. Our analysis represents IBD Movement’s perspective and is intended to help patients understand how this news may affect them. Read the original article for complete details.
What This Means for the IBD Community
This discovery feels different from other research we’ve seen, and here’s why it matters so much for our community. For years, many of us have felt like our Crohn’s symptoms were unpredictable and mysterious. We’ve tried elimination diets, tracked our foods obsessively, and still couldn’t pinpoint exactly why some days are good and others are terrible.
This hydrogen engine research gives us a concrete, measurable mechanism that could explain some of that unpredictability. It’s not just “inflammation”—it’s a specific bacterial imbalance that we can potentially identify and address.
From a practical standpoint, this could change how we approach Crohn’s management in several ways:
- Better diagnostic tools: Instead of relying solely on colonoscopies and blood tests, doctors might soon be able to test the hydrogen-processing capacity of your gut bacteria to better understand your specific condition.
- Personalized treatment approaches: Rather than the current one-size-fits-all medication approach, treatments could be tailored based on your individual bacterial hydrogen engine status.
- New therapeutic targets: This opens the door for treatments specifically designed to restore these hydrogen-consuming bacteria or support their function.
What’s particularly exciting is that this research aligns with what many of us have experienced with probiotics and dietary changes. Some people with Crohn’s report improvement with certain probiotic strains—and now we might understand why. Those probiotics could be helping to restore the hydrogen-processing bacteria that are missing or reduced in our guts.
This also validates the experiences of patients who’ve found relief through fecal microbiota transplantation (FMT). While FMT isn’t widely available for Crohn’s yet, this research suggests that transplanting healthy bacterial communities—including those hydrogen-consuming bacteria—could indeed be therapeutic.
Questions to Consider for Your Next Doctor Visit
If this research resonates with you, here are some thoughtful questions you might want to discuss with your gastroenterologist:
- Are there currently any tests available to assess the hydrogen-processing capacity of my gut bacteria?
- How might this research influence my current treatment plan or medication choices?
- Should I be considering specific probiotic strains that might help restore hydrogen-consuming bacteria?
- Are there any clinical trials related to this hydrogen engine research that I might be eligible for?
It’s worth noting that this is still early-stage research, so don’t expect immediate changes to standard treatment protocols. However, being aware of these developments can help you have more informed discussions with your healthcare team and potentially explore complementary approaches that align with this research.
The Bigger Picture for IBD Research
This discovery fits into a broader trend we’re seeing in IBD research—a move away from treating Crohn’s as just an immune system problem and toward understanding it as a complex ecosystem disruption. We’re seeing similar approaches in other areas of medicine, where researchers are looking at the interplay between our human cells and the trillions of bacteria that call our bodies home.
What gives me hope about this particular research is its specificity. We’re not just talking about “gut bacteria are important”—we’re talking about a specific metabolic pathway (hydrogen processing) and specific types of bacteria (hydrogenotrophs) that have measurable functions. This kind of precision is what leads to targeted, effective treatments.
This research also highlights something our community knows well: our guts are incredibly complex ecosystems, and healing often requires supporting that entire ecosystem rather than just suppressing symptoms. It validates the holistic approaches that many patients have found helpful, while providing a scientific framework for understanding why they work.
Looking Ahead: Reasons for Optimism
While we shouldn’t expect overnight changes, this research opens several promising avenues. The most immediate possibility is the development of diagnostic tests that could help doctors better understand each patient’s specific bacterial imbalances. This could lead to more personalized treatment approaches—something our community desperately needs.
Longer term, we might see new probiotic formulations specifically designed to restore hydrogen-consuming bacteria, or even engineered bacteria that are particularly effective at hydrogen processing. The research also strengthens the case for fecal microbiota transplantation as a legitimate treatment option for Crohn’s disease.
Perhaps most importantly, this research reminds us that our bodies want to heal. The hydrogen engine system works beautifully in healthy people—it’s not broken by design, it’s disrupted by disease. This suggests that with the right interventions, we can potentially restore this natural balance and help our bodies remember how to maintain digestive health.
For all of us living with Crohn’s, this discovery represents hope grounded in solid science. It’s not a miracle cure, but it’s a meaningful step toward understanding the biological mechanisms that drive our condition. And understanding, as we all know, is the first step toward more effective treatment and, hopefully, better days ahead.
IBD Movement provides information for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.







