Understanding ‘Creeping Fat’: The Hidden Factor in Crohn’s Complications
There’s something quietly unsettling about learning that your own body might be working against you in ways you never imagined. If you’re living with Crohn’s disease, you’re already familiar with the unpredictable nature of inflammation, the careful dance around trigger foods, and the constant vigilance required to manage symptoms. But what if there’s another player in this complex game—one that’s been hiding in plain sight, literally wrapping itself around your intestines?
That’s exactly what researchers are discovering about something called “creeping fat,” and while the name might sound almost fictional, its impact on Crohn’s disease is very real. For those of us in the IBD community, understanding this phenomenon could be a crucial piece of the puzzle in comprehending why some people develop strictures and complications while others don’t.
Summary of research findings
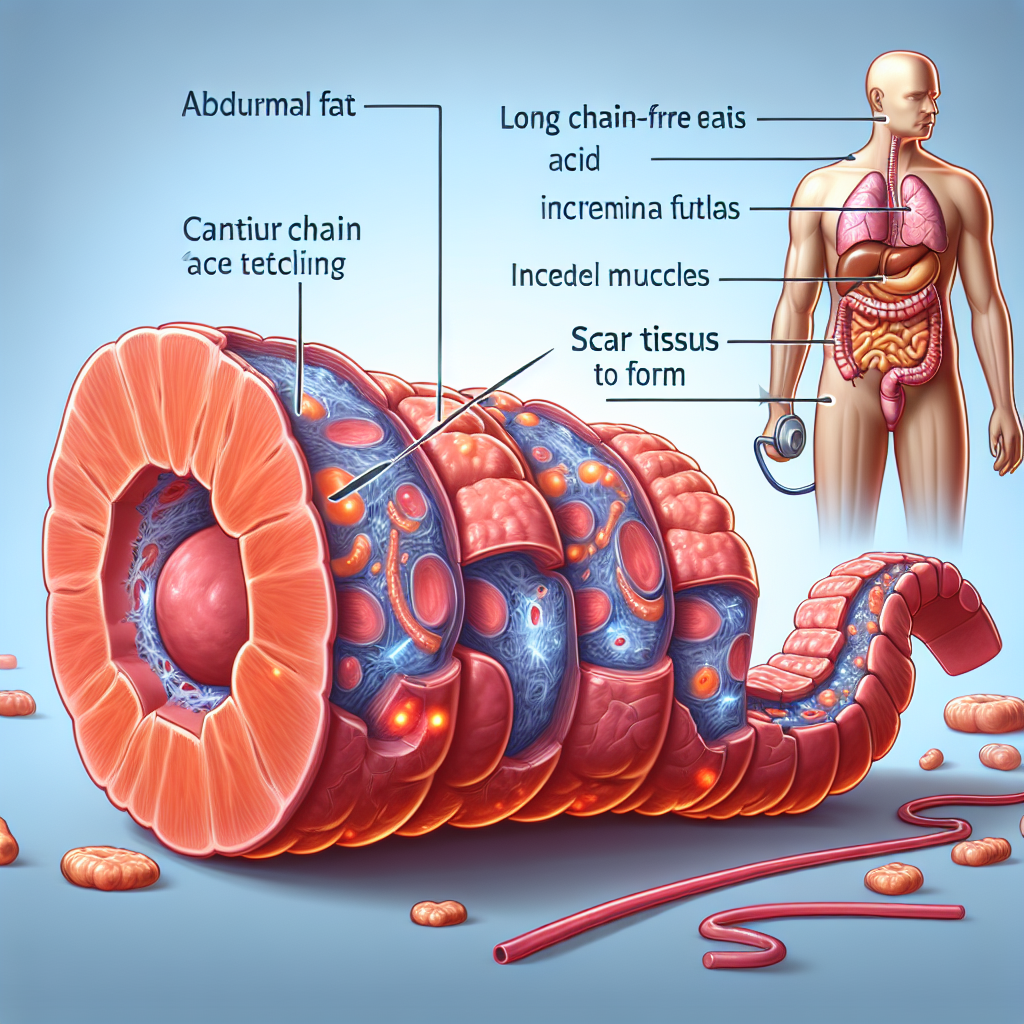
Scientists have identified a specific type of fat tissue that develops around the intestines in people with Crohn’s disease, aptly named “creeping fat” because of how it literally creeps around the bowel. Unlike regular fat tissue that simply stores energy, this fat behaves more like an active participant in the disease process.
Research has shown that creeping fat isn’t just sitting passively—it’s actively contributing to complications. This tissue releases specific fatty acids and inflammatory signals that encourage the intestinal muscles to thicken and overgrow. This process leads to scarring and the formation of strictures (narrowed areas of the intestine) that can cause blockages and often require surgical intervention.
In laboratory studies with mice, researchers found that when they blocked the influence of this creeping fat, they could reduce the dangerous muscle thickening that leads to strictures. Currently, there are no medications specifically designed to target this fat tissue, but this research is opening up new possibilities for treatment approaches.
The relationship between dietary fats and IBD is also complex—while some fats from processed foods may increase IBD risk, others like omega-3 fatty acids might actually provide protection against inflammation.
What This Means for the IBD Community
As someone who’s spent years helping people navigate life with IBD, I find this research both fascinating and deeply meaningful for our community. First, it validates what many of you have suspected all along—that Crohn’s disease involves more than just inflammation of the intestinal lining. There are multiple biological processes at work, some of which we’re only beginning to understand.
For those who’ve experienced strictures or required surgery for blockages, this research provides important context. It’s not just “bad luck” or poor disease management—there may be specific biological mechanisms like creeping fat contributing to these complications. This understanding can help reduce the self-blame that many patients carry when their disease progresses despite their best efforts to manage it.
From a practical standpoint, this research highlights why regular monitoring with your gastroenterologist is so crucial. While we can’t yet directly treat creeping fat, understanding that it exists and contributes to stricture formation makes imaging studies like CT scans or MRIs even more valuable. These tests can help your medical team identify areas where creeping fat is developing and monitor for early signs of stricture formation.
The dietary implications are particularly relevant for daily life with IBD. While the research shows that different types of fats can have opposite effects on inflammation, this doesn’t mean you need to fear all fats or obsess over every dietary choice. Instead, it reinforces the importance of working with a dietitian who understands IBD to develop an eating plan that supports your overall health while minimizing inflammation.
This research also raises important questions you might want to discuss with your doctor: Are there imaging signs that suggest creeping fat development in your case? How does your current treatment plan address not just inflammation but also the mechanical complications that can arise? Should you be considering any dietary modifications based on this research?
Perhaps most importantly, this discovery represents hope for future treatment options. While current IBD medications focus primarily on controlling inflammation, understanding the role of creeping fat opens the door to entirely new therapeutic approaches. Imagine treatments that could prevent strictures from forming in the first place, rather than waiting to address them after they’ve already caused problems.
This research also connects to broader trends we’re seeing in IBD care—the move toward more personalized, precision medicine. As we better understand the various biological pathways involved in Crohn’s disease, we’re getting closer to treatments that can be tailored to each person’s specific disease patterns and risk factors.
For caregivers and family members, this information helps explain why IBD management can be so complex and why complications sometimes develop despite everyone’s best efforts. It’s not about doing something wrong—it’s about managing a multifaceted disease that involves numerous biological processes we’re still working to understand.
Looking Ahead: Questions and Possibilities
While this research is promising, it also raises important questions that future studies will need to address. How can we identify people who are most likely to develop problematic creeping fat? Are there lifestyle factors that influence its development? Could existing medications have unrecognized effects on this tissue?
The connection between diet and creeping fat development is particularly intriguing. While we know that certain dietary patterns can influence IBD risk and outcomes, understanding how specific fats might contribute to or protect against creeping fat formation could lead to more targeted dietary recommendations for people with Crohn’s disease.
There’s also the question of timing—when does creeping fat typically develop in the disease course? If we can identify it early, might we be able to intervene before it causes significant problems? These are the kinds of questions that could transform how we approach Crohn’s disease management.
For those living with IBD today, while we wait for these targeted therapies to be developed, the best approach remains comprehensive disease management with your healthcare team. This includes staying on top of anti-inflammatory treatments, monitoring for complications, maintaining good nutrition, and advocating for the care you need.
Understanding creeping fat also reinforces why it’s so important to maintain open communication with your medical team about any new or changing symptoms. Stricture-related symptoms like persistent abdominal pain, bloating after meals, or changes in bowel habits should always be evaluated promptly, as early intervention can often prevent more serious complications.
This research represents more than just another scientific discovery—it’s a window into the complex biology of IBD that brings us closer to more effective, personalized treatments. While we may not have medications to target creeping fat today, understanding its role gives us hope for a future where strictures and their complications could become far less common for people with Crohn’s disease. That’s the kind of progress that makes all the research worthwhile, and it’s why staying informed about these developments matters so much for our community.
IBD Movement provides information for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.







