The Hidden Path: My Journey Through Fistula Diagnosis and Fistulectomy Recovery
This story represents a composite of common IBD experiences and is presented to help readers feel less alone in their journey.
The Uncomfortable Truth
I’ll never forget the moment I finally said the words out loud to my gastroenterologist: “I think something is draining from places it shouldn’t be.” My face burned with embarrassment as I described the persistent, foul-smelling discharge that had been plaguing me for months. At 34, I’d been living with Crohn’s disease for eight years, but this was different—this was something I couldn’t bring myself to Google or mention in my IBD support group. The shame felt almost worse than the physical discomfort.
Dr. Martinez listened without judgment as I stumbled through my explanation, her expression growing more serious with each detail. “Sarah, what you’re describing sounds like it could be a fistula,” she said gently. “It’s actually more common than you might think with Crohn’s disease, especially with your history of perianal involvement.”
That word—fistula—hung in the air like a diagnosis I’d been dreading without even knowing it existed.
The Beginning: When Normal Became Abnormal
Looking back, the signs had been there for months, but I’d convinced myself they were just part of my “normal” Crohn’s experience. It started with what I thought was just another flare-up—increased pain around my tailbone area, more frequent trips to the bathroom, and a general feeling that something wasn’t quite right. I’d been managing my Crohn’s relatively well for years with adalimumab, so when these new symptoms appeared, I initially attributed them to stress from a job change.
The first real sign something was different came during what should have been a routine shower. I noticed a small, tender bump near my anal area that seemed to be getting larger. Within days, it became painful to sit, and I found myself constantly shifting positions at work. Then came the drainage—a clear, sometimes bloody discharge that had an unmistakable odor.
I spent weeks researching everything except what I was actually experiencing. I convinced myself it was hemorrhoids, then a skin infection, then just “part of having Crohn’s.” The internet was simultaneously my best friend and worst enemy—I’d start to look up my symptoms, then immediately close the browser when the search results became too frightening or graphic.
The breaking point came when I developed a fever and the pain became unbearable. My husband practically had to drag me to the emergency room, where a young resident took one look and said, “This looks like a perianal abscess. We need to get surgery involved.” That night, I had my first drainage procedure, but it wasn’t until weeks later that we discovered the deeper problem: the abscess had formed because of an underlying fistula tract.
The Struggle: Living in the Shadows
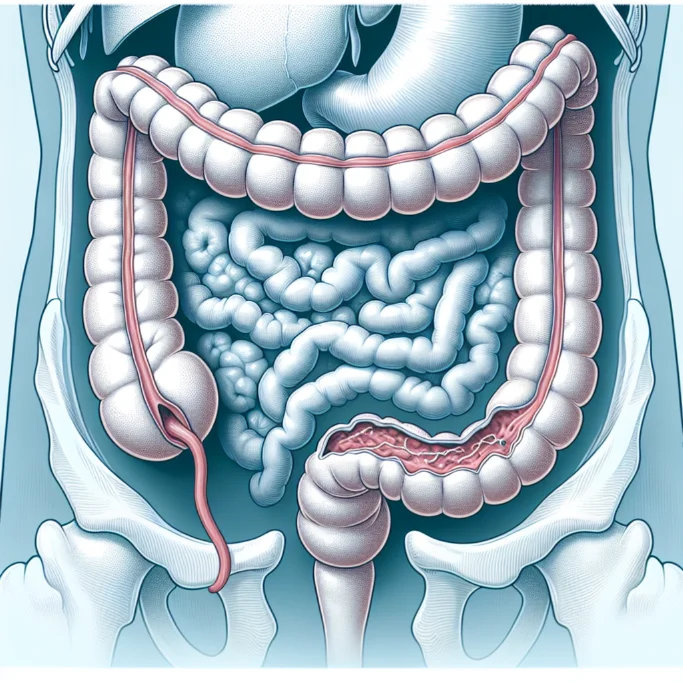
The months following my abscess drainage were some of the most challenging of my entire IBD journey, and that’s saying something. The fistula diagnosis came after an MRI that revealed a complex tract connecting my intestine to the skin surface—essentially, a tunnel that shouldn’t exist, allowing intestinal contents to leak where they had no business being.
What made this period particularly difficult wasn’t just the physical symptoms, though those were significant. The constant drainage meant I had to wear pads constantly, changing them multiple times a day. The smell was something I became hyperaware of, convinced that everyone around me could detect it. I started declining social invitations, avoiding the gym, and even reconsidering intimate moments with my husband.
The treatment options my colorectal surgeon presented were overwhelming and frankly terrifying. “We could try a seton placement first,” Dr. Chen explained, “which is essentially a surgical thread that keeps the tract open to allow healing from the inside out. If that doesn’t work, we might need to consider a fistulectomy—surgically removing the entire tract.”
I chose to try the seton first, but after six months of living with what felt like a permanent surgical drain, the tract hadn’t healed. The decision to move forward with a fistulectomy felt both inevitable and terrifying. How do you explain to your boss that you need time off for surgery on such a private area? How do you tell friends why you can’t sit comfortably for weeks?
The pre-surgical period was filled with uncomfortable conversations and preparations I’d never imagined needing. The surgeon explained the risks: potential incontinence, delayed healing, possible recurrence. My IBD had taught me to advocate for myself, but discussing anal function and surgical risks felt like crossing into territory I wasn’t equipped to handle.
What struck me most was the silence surrounding this condition. Unlike other aspects of IBD that had active online communities and support groups, fistulas felt like a taboo subject even within the Crohn’s community. I felt incredibly alone, which made the decision-making process even more daunting.
The Turning Point: Finding My Voice and My Team
The turning point came not from the surgery itself, but from a conversation with my IBD nurse, Janet, two weeks before my scheduled fistulectomy. I’d been sitting in the infusion center, getting my regular adalimumab injection, when she noticed I seemed particularly anxious.
“You know,” she said quietly, “about 30% of people with Crohn’s develop fistulas at some point. You’re not alone in this, and there’s nothing to be ashamed of.” She then did something that changed everything—she connected me with another patient who had been through a similar experience.
Meeting Maria, a 42-year-old teacher who had undergone a fistulectomy two years earlier, was revelatory. She spoke openly about the challenges, the recovery process, and most importantly, about how her life had improved afterward. “The hardest part,” she told me, “was the secrecy and shame I put on myself. The actual surgery and recovery were manageable once I stopped trying to hide from it.”
Armed with this new perspective, I approached my fistulectomy with a different mindset. I had honest conversations with my husband about what recovery would look like. I spoke frankly with my surgeon about my concerns and expectations. I even told my closest friends what I was going through, and their support surprised me with its warmth and lack of judgment.
The surgery itself was performed as an outpatient procedure under general anesthesia. Dr. Chen removed the entire fistula tract and closed the internal opening. I woke up with surgical packing that would need to be changed daily—another aspect of recovery I hadn’t fully prepared for mentally, but was now ready to handle practically.
Living Well Today: Embracing the New Normal
Eighteen months post-fistulectomy, I can honestly say that having the surgery was one of the best decisions I’ve made for my health. The recovery wasn’t easy—six weeks of daily wound care, sitz baths three times a day, and careful attention to hygiene became my routine. But each week brought noticeable improvement.
The most significant change has been the absence of constant worry about drainage and odor. I can wear whatever underwear I want without thinking about protection. I can sit through long meetings without discomfort. I can be intimate with my husband without the anxiety that had been shadowing our relationship for months.
My daily routine now includes some ongoing management strategies that have become second nature. I’m more vigilant about my Crohn’s management, knowing that better disease control reduces my risk of developing new fistulas. I use a bidet for gentle cleansing, maintain a high-fiber diet when my Crohn’s allows it, and stay in close communication with both my gastroenterologist and colorectal surgeon.
Perhaps most importantly, I’ve learned to speak openly about this experience. When newer members join my IBD support group and mention mysterious symptoms they’re embarrassed to discuss, I share my story. I’ve become the person I needed when I was struggling in silence.
The follow-up care has been crucial to my success. Regular check-ups with my colorectal surgeon, MRI scans to monitor for recurrence, and ongoing optimization of my Crohn’s medications have all played a role in my continued healing. My surgical site healed completely within three months, and there’s been no sign of recurrence.
A Message of Hope and Healing
If you’re reading this because you’re facing a fistula diagnosis or considering a fistulectomy, please know that you’re not alone, and there’s nothing shameful about your condition. Fistulas are a recognized complication of Crohn’s disease, affecting nearly one in three of us at some point. They’re not a reflection of anything you’ve done wrong or failed to do right.
The diagnosis process can be challenging because fistulas don’t always present in textbook ways, and many of us delay seeking help due to embarrassment. If you’re experiencing unusual drainage, persistent pain in the perianal area, or recurrent abscesses, please don’t wait as long as I did to speak up. Your healthcare team has seen this before, and they’re equipped to help you navigate both the diagnosis and treatment options.
Fistulectomy isn’t the right choice for everyone, and it’s not always the first treatment option, but for those who do undergo the procedure, the outcomes are often very positive. The key is finding a colorectal surgeon experienced in IBD-related fistulas and being honest about your concerns and expectations.
Most importantly, don’t let shame keep you from seeking the help you deserve. The IBD community is stronger when we support each other through all aspects of this disease, including the ones that feel too private or embarrassing to discuss. Your story matters, your healing matters, and your willingness to speak up might be exactly what someone else needs to hear.
Today, I live without the constant worry and discomfort that defined those difficult months. The surgery gave me back not just physical comfort, but also the confidence to live fully with my Crohn’s disease. That’s a gift worth every uncomfortable conversation and every day of recovery.







