Silent Liver Warnings: What IBD Patients Need to Know
When you live with Crohn’s disease or ulcerative colitis, your relationship with your body becomes complicated. You learn to distinguish between your usual IBD symptoms and something else—but what happens when new warning signs disguise themselves as familiar discomfort? For those of us managing inflammatory bowel disease, understanding the subtle signs of liver problems becomes even more crucial, especially when certain IBD medications can affect liver function.
Living with chronic illness teaches you to be hypervigilant about changes in your body, yet sometimes the most important signals whisper rather than shout. Your liver might be trying to tell you something important, but are you listening?
Summary of Read the full story here
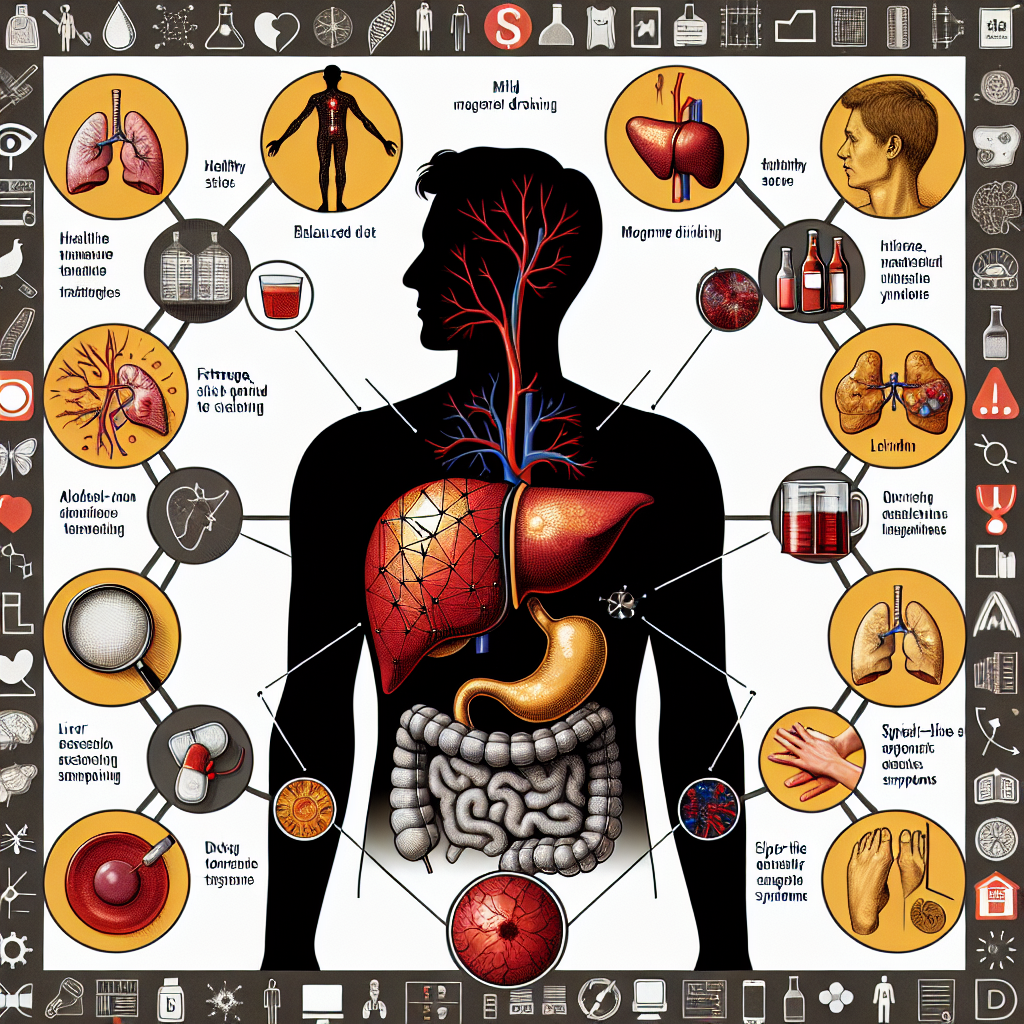
Recent reporting highlights how liver disease often begins with symptoms that many people dismiss as everyday fatigue or stress. The early warning signs include persistent tiredness, unexplained nausea, and a dull ache under the ribs—symptoms that can easily be attributed to other causes. Many individuals remain unaware of their risk until routine medical tests reveal developing liver problems.
The article emphasizes that family history and lifestyle factors play significant roles in liver disease risk. Early detection is crucial because it opens doors to treatment options that become less effective as the disease progresses. Healthcare advocates stress the importance of community support and sharing experiences to help people recognize these subtle warning signs before they become serious health threats.
This post summarizes reporting from Read the full story here. Our analysis represents IBD Movement’s perspective and is intended to help patients understand how this news may affect them. Read the original article for complete details.
What This Means for the IBD Community
For those of us living with IBD, this information carries special significance. Our bodies are already working overtime to manage chronic inflammation, and certain medications we rely on—including some immunosuppressants like azathioprine, methotrexate, and even prolonged steroid use—require regular liver function monitoring. This makes us uniquely positioned to catch liver problems early, but it also means we need to be extra vigilant.
The tricky part? Many early liver disease symptoms overlap with what we might consider “normal” IBD experiences. That persistent fatigue could be from poor sleep due to nighttime bathroom trips, or it could be your liver signaling for help. Nausea might seem like a flare-up symptom, but paired with other signs, it could indicate something more serious.
Here’s what makes this particularly relevant for our community: IBD patients already have a higher baseline risk for certain liver complications. Primary sclerosing cholangitis (PSC), for instance, occurs in about 2-8% of people with ulcerative colitis. Additionally, the chronic inflammation that defines IBD can sometimes affect other organs, including the liver.
Red Flags That Deserve Immediate Attention
While we’re used to monitoring our symptoms, certain combinations should prompt an urgent conversation with your gastroenterologist or hepatologist:
- Persistent fatigue that doesn’t improve with better sleep or IBD symptom management
- Nausea accompanied by loss of appetite, especially if it’s different from your usual IBD-related nausea patterns
- Abdominal pain in the upper right quadrant (different from typical IBD cramping)
- Yellowing of the skin or eyes (jaundice)
- Dark-colored urine combined with pale stools
- Unexplained weight loss beyond what you’d expect from an IBD flare
The key is recognizing patterns that feel different from your usual IBD experience. You know your body better than anyone—trust those instincts when something feels “off” in a new way.
Medication Monitoring: Your Safety Net
If you’re taking IBD medications that require liver monitoring, those regular blood tests are actually your early warning system. Liver enzymes like ALT and AST can reveal problems before you feel any symptoms. Don’t skip these appointments, even when you’re feeling well. Many IBD patients have discovered liver issues through routine monitoring that might otherwise have gone unnoticed for months or years.
Your healthcare team likely already has protocols in place, but it’s worth discussing your individual risk factors. Do you have a family history of liver disease? Have you had hepatitis? Do you drink alcohol regularly? These conversations help your doctor tailor monitoring to your specific needs.
The Community Connection
One of the most powerful aspects of the IBD community is how we share experiences and look out for each other. This extends beyond typical IBD symptoms to encompass all aspects of our health journey. When someone mentions feeling “different tired” or experiencing new symptoms, those conversations in support groups, forums, and social media can be life-saving.
Consider being part of this protective network. Share your experiences with medication monitoring, discuss how you distinguish between different types of symptoms, and listen when others describe changes in their health. Sometimes an outside perspective helps us recognize patterns we’re too close to see ourselves.
Questions for Your Next Appointment
Armed with this information, here are important questions to bring up during your next gastroenterology visit:
- Given my IBD medications and history, what’s my personal risk for liver complications?
- How often should my liver function be monitored, and what specific tests should I expect?
- What symptoms should prompt me to call your office immediately versus waiting for my next scheduled visit?
- Are there any interactions between my IBD medications and other drugs that could affect my liver?
- Should I be seeing a hepatologist in addition to my gastroenterologist?
These aren’t questions that suggest you don’t trust your current care—they demonstrate that you’re an engaged, informed patient who understands the interconnected nature of your health.
Taking Control Without Taking Over
Living with IBD teaches us to balance vigilance with living our lives. The same principle applies to liver health awareness. You don’t need to become anxious about every symptom, but you do need to stay informed and communicative with your healthcare team.
Keep a simple symptom journal if it helps you identify patterns. Note when you feel unusually tired, any changes in appetite or nausea, and how these symptoms relate to your IBD management. This information becomes invaluable during medical appointments and helps distinguish between IBD-related issues and potential liver concerns.
Regular self-advocacy is key. If you notice the subtle warning signs mentioned in the reporting—that persistent fatigue, unexplained nausea, or discomfort under your ribs—don’t dismiss them as “just IBD.” Your body deserves the same attention you’d give to recognizing an IBD flare.
Living with chronic illness means we become experts in our own bodies, but it also means we can sometimes normalize symptoms that deserve medical attention. This balance requires ongoing mindfulness and the courage to speak up when something feels different, even if we can’t quite put our finger on what’s changed.
The liver’s silent nature means early detection often depends on routine monitoring and paying attention to subtle changes. For IBD patients, this vigilance is already built into our healthcare routine through medication monitoring and regular specialist visits. We have the infrastructure in place—we just need to use it effectively and trust our instincts when something feels off.
Your IBD journey has already taught you to be your own advocate. Apply those same skills to your overall health, including liver function. The combination of regular medical monitoring, community support, and personal awareness creates a powerful early detection system that can catch problems when they’re still manageable.
Remember, catching liver problems early doesn’t just mean better treatment options—it means maintaining your quality of life and continuing to manage your IBD effectively. When all your organs are functioning well together, your overall health improves, often making IBD management easier too.
This interconnected approach to health management represents the best of what we’ve learned from living with IBD: stay informed, stay connected to your healthcare team and community, and never hesitate to advocate for yourself when something doesn’t feel right. Your liver—and your overall health—will thank you for this proactive approach.
IBD Movement provides information for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.







