IL-22: The Body’s Helper That Sometimes Hurts IBD Patients
When you’re living with Crohn’s disease or ulcerative colitis, every new research discovery feels personal. We’re always searching for answers to why our bodies seem to turn against us, why treatments work differently for each of us, and what might finally lead to better days ahead.
Recently, I’ve been following research that’s uncovering something fascinating about our immune systems—and it’s both hopeful and complex in that way IBD research often is. Scientists are learning more about a protein called interleukin-22 (IL-22) that plays a surprising double role in inflammatory bowel disease, and understanding it might help explain why some of us experience more severe symptoms than others.
Summary of A New Clue in IBD: Blood Protein IL-22 Linked to Worse Symptoms in Crohn’s and Colitis
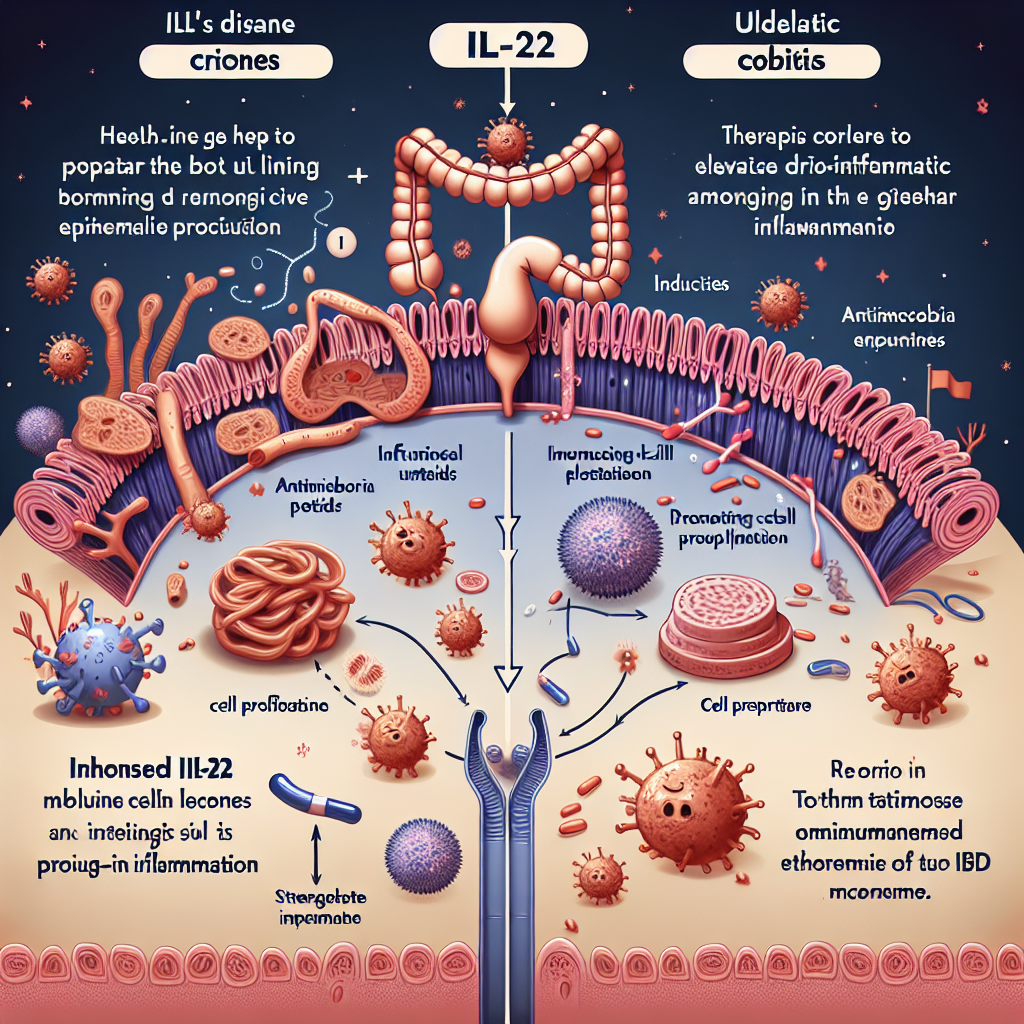
Researchers have identified that IL-22, a protein produced by our immune system, acts like a double-edged sword in IBD. On the positive side, IL-22 helps heal the gut lining, fights off infections, and repairs damage to our intestines. However, when IL-22 levels remain elevated over time—particularly in chronic conditions like Crohn’s and colitis—it appears to fuel the very inflammation it was designed to control.
Studies show that people with more severe IBD symptoms tend to have higher levels of IL-22 in both their blood and gut tissue. The protein triggers the expression of another molecule called OSMR, which can keep the gut in a pro-inflammatory state, creating a cycle of ongoing tissue irritation and immune system overdrive. Laboratory experiments demonstrated that when IL-22 was blocked, harmful inflammation decreased and gut tissue began to heal more effectively.
This post summarizes reporting from A New Clue in IBD: Blood Protein IL-22 Linked to Worse Symptoms in Crohn’s and Colitis. Our analysis represents IBD Movement’s perspective and is intended to help patients understand how this news may affect them. Read the original article for complete details.
What This Means for the IBD Community
This IL-22 research represents something I find both exciting and deeply relevant to our daily experiences with IBD. Think about those moments when you’re feeling relatively well, but then something seems to tip the scales toward a flare. We often blame stress, diet, or medication changes—and those factors certainly matter—but this research suggests there might also be molecular-level processes happening that we’re just beginning to understand.
The concept of IL-22 as a “helper gone rogue” resonates with how many of us experience IBD. Our immune systems are supposed to protect us, but in IBD, that same protective mechanism becomes our biggest challenge. IL-22 perfectly exemplifies this paradox: it’s trying to heal our gut, but when it overstays its welcome, it ends up making things worse.
For those of us who’ve wondered why we seem to have more severe symptoms than others with the same diagnosis, IL-22 levels might provide part of the explanation. This isn’t about fault or blame—it’s about biology and individual variation. Some people might naturally produce more IL-22, or their bodies might not regulate it as effectively, leading to more persistent inflammation.
Practical implications for patients: While we can’t currently test our IL-22 levels at home or ask for them in routine blood work, understanding this mechanism can help us have more informed conversations with our healthcare teams. If you’re someone who experiences particularly stubborn inflammation despite treatment, IL-22 pathways might be worth discussing as a potential factor.
This research also validates what many of us have long suspected: IBD is incredibly complex, and one-size-fits-all treatments don’t work because our individual immune responses vary significantly. The IL-22 findings support the movement toward personalized medicine, where treatments are tailored to each person’s specific inflammatory patterns.
Questions to consider discussing with your doctor:
- Could elevated inflammation markers in my blood tests be related to proteins like IL-22?
- Are there emerging treatments targeting specific inflammatory pathways like IL-22?
- How might understanding my individual inflammatory profile help optimize my treatment plan?
- What role might IL-22 play in my treatment resistance or persistent symptoms?
The research also connects to broader trends we’re seeing in IBD treatment development. Pharmaceutical companies are increasingly focusing on targeted therapies that address specific inflammatory pathways rather than broadly suppressing the immune system. The challenge with IL-22, as the research shows, is finding that sweet spot—reducing harmful inflammation while preserving the protein’s beneficial healing properties.
This represents the kind of nuanced approach that IBD treatment desperately needs. Too often, we’ve had to choose between medications that might help inflammation but compromise our immune system’s ability to fight infections, or accept ongoing inflammation to maintain some immune function. Understanding molecules like IL-22 could lead to more precise interventions.
From a caregiver perspective, this research offers valuable insight into why IBD can be so unpredictable. When someone you love is managing Crohn’s or colitis, it can be frustrating not to understand why good days turn into bad days seemingly without warning. Learning about proteins like IL-22 helps explain that sometimes, the body’s own healing mechanisms can become part of the problem—it’s not about anything the person did wrong.
Looking Toward Future Treatments
What excites me most about this IL-22 research is the potential for developing smarter treatments. Instead of broadly suppressing inflammation, future therapies might be able to modulate IL-22 activity more precisely. Imagine treatments that could dial down IL-22’s inflammatory effects while preserving its healing benefits—that would be a game-changer for many of us.
The research timeline for translating these discoveries into actual treatments is always longer than we’d like, but having clearer targets like IL-22 accelerates the development process. Drug companies can now design clinical trials specifically testing IL-22 modulators, rather than taking the broader approach that’s characterized much of IBD treatment development in the past.
The bottom line: This IL-22 research gives us another piece of the IBD puzzle, and every piece brings us closer to better treatments and deeper understanding. While we can’t change our IL-22 levels today, knowing about this mechanism helps validate our experiences and points toward more personalized approaches to managing IBD. It’s exactly the kind of targeted research that makes me optimistic about the future of IBD care—complex problems require sophisticated solutions, and scientists are rising to meet that challenge.
Most importantly, this research reminds us that the severity of our symptoms isn’t a reflection of our willpower or self-care efforts. Sometimes, it’s about proteins like IL-22 doing their job a little too enthusiastically. Understanding that can be both reassuring and empowering as we continue advocating for our health and working with our medical teams to find the best path forward.
IBD Movement provides information for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.







