The Tooth About IBD: How My Dental Health Nearly Destroyed My Remission
This story represents a composite of common IBD experiences and is presented to help readers feel less alone in their journey.
The Throbbing Wake-Up Call
The pain hit me at 3 AM like a lightning bolt straight to my jaw. I’d been managing my Crohn’s disease successfully for two years on methotrexate and Humira, finally feeling like I had my life back. But as I sat in my bathroom, clutching my swollen face and watching blood swirl in the sink after brushing my teeth, I had no idea that this dental emergency was about to unravel everything I’d worked so hard to achieve.
What started as a minor toothache three days earlier had escalated into a full-blown abscess. My left cheek looked like I was storing a golf ball, and the metallic taste in my mouth told me the infection was spreading. But here’s what terrified me most: within hours of that sleepless night, I felt the familiar cramping in my abdomen that signaled an impending Crohn’s flare. The connection between my mouth and my gut was about to teach me a lesson no doctor had ever mentioned.
When Two Worlds Collide
My journey with Crohn’s disease began five years ago, and like many patients, I became laser-focused on managing my digestive symptoms. My gastroenterologist and I had found the perfect combination of medications, and my regular colonoscopies showed beautiful, healed tissue. I thought I had this disease figured out. What no one had told me was that the very medications keeping my intestines calm were setting up a perfect storm in my mouth.
The first sign should have been the persistent mouth ulcers that started appearing about six months after beginning methotrexate. I mentioned them to my GI doctor, who nodded and said they were “common” but didn’t elaborate on the implications. My dentist noticed my gums bleeding more during cleanings, but attributed it to stress. Neither specialist seemed to understand how these issues were connected to my overall IBD management.
The real wake-up call came when I developed that severe dental abscess. What I didn’t know then was that methotrexate, which suppresses my immune system to control intestinal inflammation, also dramatically slows wound healing in my mouth. That small cavity I’d been putting off treating had become a breeding ground for bacteria that my compromised immune system couldn’t fight off effectively.
The Perfect Storm: When Dental Infections Trigger IBD Flares
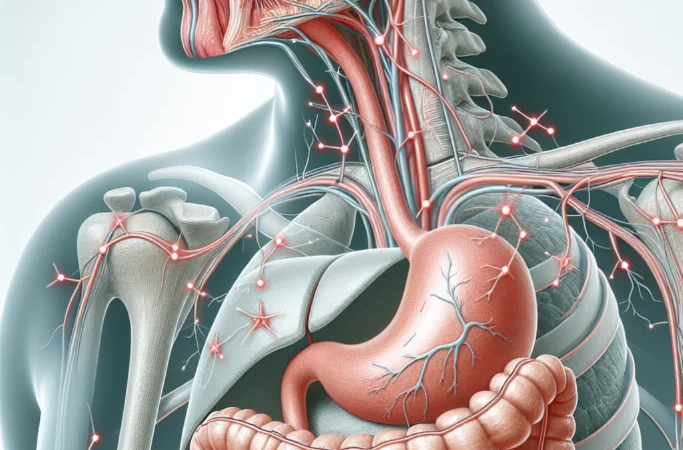
The emergency dentist who saw me that morning was the first healthcare provider to connect the dots. As he examined my swollen, infected jaw, he asked about my medications and IBD history. “This abscess is pumping inflammatory cytokines directly into your bloodstream,” he explained. “Your body is in full inflammatory mode, which can absolutely trigger an IBD flare.”
He was right. By that afternoon, I was experiencing the worst Crohn’s symptoms I’d had in two years. The cramping, the urgent bathroom trips, the fatigue – it all came rushing back. The systemic inflammation from my dental infection had essentially overridden my carefully managed IBD treatment. It was like watching dominoes fall: dental infection led to systemic inflammation, which triggered intestinal inflammation, which caused a full IBD flare.
But the nightmare was just beginning. The emergency extraction I needed couldn’t be performed immediately because of my immunosuppressive medications. The oral surgeon insisted on a specific antibiotic protocol before any procedure – something called antibiotic prophylaxis that I’d never heard of. Apparently, people on biologics like Humira are at significantly higher risk for serious infections during dental procedures, and there are special protocols that should be followed.
The most frustrating part was the communication breakdown between my medical team. My gastroenterologist knew I was on immunosuppressants but had never discussed dental implications. My dentist knew about my bleeding gums but didn’t understand the medication connections. The oral surgeon was the first to explain that IBD patients on methotrexate and biologics need coordinated care between dental and medical providers.
During the week it took to coordinate my care and get the infection under control, my Crohn’s flare worsened. I ended up needing a course of prednisone – my first steroid treatment in three years – just to get my intestinal inflammation back under control. The irony wasn’t lost on me: the medications that had given me my life back had also made me vulnerable to dental problems that could take it all away again.
Learning to Bridge Two Worlds
The turning point came when I found a dentist who specialized in medically complex patients. Dr. Martinez had experience with IBD patients and understood the intricate relationship between oral health and systemic inflammation. She became my advocate and educator, helping me understand what I wish I’d known from the beginning.
She explained that people with IBD are already at higher risk for oral health problems due to nutritional deficiencies, medication side effects, and the inflammatory nature of our disease. Add immunosuppressive medications to the mix, and we’re dealing with delayed healing, increased infection risk, and the potential for dental problems to trigger systemic flares.
Dr. Martinez introduced me to a pre-procedure protocol that has become my new normal. Before any dental work – even routine cleanings – I now follow a specific antibiotic regimen coordinated between her office and my gastroenterologist. We’ve established clear communication channels, and both providers understand my complete medical picture.
The revelation that changed everything was understanding that my mouth is essentially the gateway to my digestive system. Chronic gum disease, untreated cavities, and oral infections don’t stay localized – they create systemic inflammation that can directly impact IBD control. This connection explained so much about some of my previous “mystery flares” that we’d attributed to stress or diet.
My New Normal: Integrated Care
Today, managing my dental health is as important to my IBD care as taking my medications or following my diet. I see Dr. Martinez every three months instead of the standard six-month intervals. We do more frequent X-rays to catch problems early, before they can develop into infections that might trigger flares.
My daily routine now includes specialized mouth rinses designed for immunocompromised patients, and I use an electric toothbrush with extra-soft bristles to protect my sensitive gums. I’ve learned to recognize the early signs of oral problems – increased bleeding, persistent sores, or unusual pain – and I address them immediately rather than hoping they’ll resolve on their own.
The coordination between my healthcare providers has become seamless. My gastroenterologist now asks about my dental health at every appointment, and my dentist reviews my current IBD medications and disease activity before planning any treatments. We’ve developed a system where any significant dental work is planned around my IBD care, avoiding procedures during active flares when possible.
I’ve also become more proactive about nutrition, focusing on foods that support both gut and oral health. Vitamin D, calcium, and B vitamins are particularly important for IBD patients, and deficiencies in these nutrients can worsen oral health problems. My team monitors my levels regularly and adjusts supplements as needed.
The most important change has been my mindset. I no longer view my mouth and my gut as separate systems that happen to coexist in the same body. They’re intimately connected, and caring for one means caring for both. This holistic approach has not only prevented further dental emergencies but has also contributed to better overall IBD control.
A Message of Hope for Fellow Warriors
If you’re reading this and recognizing yourself in my story, please know that you’re not alone, and it’s not too late to take control. The connection between IBD and dental health is real, significant, and manageable once you understand it. Don’t let embarrassment about dental problems or frustration with healthcare coordination prevent you from getting the integrated care you deserve.
Start by having honest conversations with both your gastroenterologist and your dentist about your complete medical picture. Ask specifically about antibiotic protocols before dental procedures, optimal oral hygiene routines for immunocompromised patients, and warning signs that require immediate attention. Most importantly, don’t treat dental problems as separate from your IBD – they’re part of the same inflammatory puzzle.
The hidden connection between IBD and dental health that so many doctors miss is actually an opportunity. When you understand and address this relationship, you’re not just preventing dental emergencies – you’re taking control of a potential trigger for IBD flares. You’re giving yourself the best chance at long-term remission and overall health.
Your mouth is not separate from your IBD journey – it’s an integral part of it. Once you embrace this truth and build the right care team around it, you’ll wonder how you ever managed your health any other way. Trust me, the peace of mind that comes with truly integrated care is worth every extra appointment and every difficult conversation with your healthcare providers.







