Understanding the Crohn’s Disease and Joint Pain Connection: What Every Patient Should Know
Summary of WebMD
IBD Movement provides news analysis and insights for the IBD community. Always consult your healthcare provider for personal medical advice.
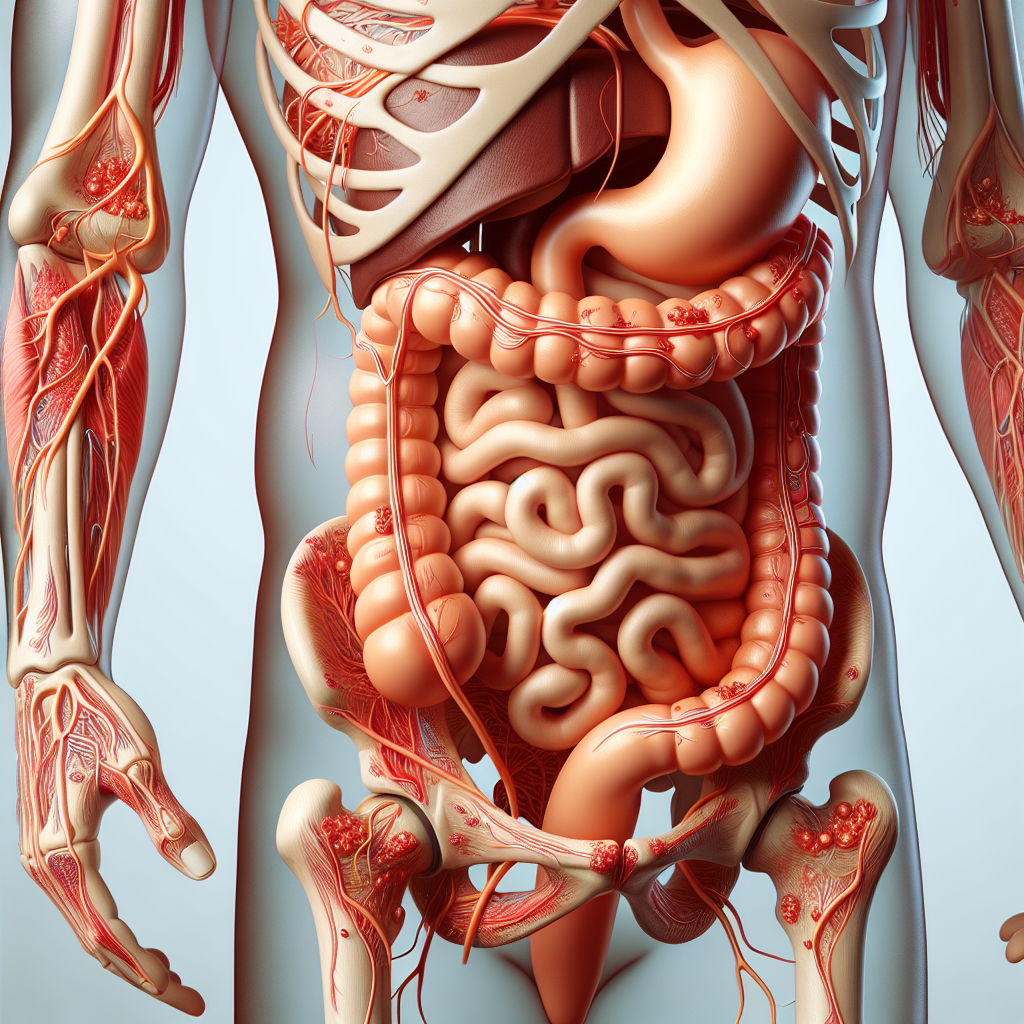
When IBD Affects More Than Your Gut
If you’re living with Crohn’s disease and experiencing unexplained joint pain, stiffness, or swelling, you’re not alone—and more importantly, you’re not imagining it. The connection between inflammatory bowel disease and joint problems affects up to 25% of people with IBD, yet many patients struggle to understand why their knees ache during a flare or why their back stiffens when their digestive symptoms worsen. This interconnection between gut inflammation and joint health represents one of the most common yet underrecognized aspects of living with Crohn’s disease, impacting not just your digestive system but your overall mobility and quality of life.
The Medical Reality Behind IBD-Related Joint Pain
According to WebMD, the relationship between Crohn’s disease and joint pain stems from the systemic inflammatory nature of IBD. When inflammation occurs in the digestive tract, it doesn’t always stay confined to the gut. The same inflammatory processes that damage intestinal tissue can trigger inflammatory responses in joints, leading to a condition known as inflammatory arthritis or IBD-associated arthropathy.
The medical literature identifies two primary types of joint involvement in Crohn’s disease: peripheral arthritis, which affects joints in the arms and legs, and axial arthropathy, which impacts the spine and pelvis. Peripheral arthritis tends to correlate directly with IBD flare-ups, often improving when intestinal inflammation is controlled. Axial involvement, however, may follow an independent course, sometimes persisting even when digestive symptoms are well-managed.
Research indicates that certain genetic factors, particularly the HLA-B27 gene, increase the likelihood of developing joint complications alongside IBD. Additionally, the severity and location of intestinal inflammation can influence joint involvement patterns, with colonic Crohn’s disease showing higher rates of peripheral arthritis compared to purely small bowel disease.
What This Connection Means for Your Daily Life with IBD
Understanding the Crohn’s-joint pain connection fundamentally changes how we approach IBD management and daily living strategies. For many patients, joint symptoms serve as an early warning system for impending digestive flares, often appearing days or weeks before abdominal symptoms intensify. This biological early warning system can be incredibly valuable for proactive treatment adjustments when patients learn to recognize these patterns.
The implications extend far beyond simple symptom recognition. Joint involvement significantly impacts treatment decisions, as medications that effectively manage intestinal inflammation may not adequately address joint symptoms, and vice versa. This dual challenge often requires a more comprehensive therapeutic approach, potentially involving gastroenterologists, rheumatologists, and physical therapists working collaboratively.
From a lifestyle perspective, joint involvement adds another layer of complexity to exercise and activity planning. While regular movement remains crucial for both digestive and joint health, the type, intensity, and timing of physical activity may need adjustment based on both IBD activity and joint symptoms. Low-impact exercises like swimming, yoga, and walking often provide the best balance of maintaining mobility without exacerbating inflammation.
The psychological impact cannot be overlooked either. Many patients describe feeling frustrated when joint pain limits activities during periods when their digestive symptoms are well-controlled. This disconnect between gut health and joint symptoms can create confusion and anxiety about disease progression, making patient education and support particularly important.
Nutritionally, the anti-inflammatory diet approaches that benefit IBD may also support joint health, creating synergistic benefits. However, some patients find that certain foods trigger joint symptoms independently of digestive reactions, requiring individualized dietary strategies that address both aspects of their condition.
Sleep quality often becomes compromised when joint pain accompanies IBD symptoms, creating a cycle where poor sleep worsens inflammation, which in turn affects both digestive and joint symptoms. Addressing sleep hygiene and pain management becomes essential for overall disease control.
The connection also influences medication adherence and treatment satisfaction. Patients experiencing joint symptoms may feel their IBD treatment is inadequate, even when digestive markers show good control. This perception can lead to treatment changes or additions that specifically target the inflammatory pathways affecting joints.
Expert Perspectives on Managing Both Conditions
Gastroenterologists and rheumatologists increasingly recognize the need for integrated care approaches when treating IBD patients with joint involvement. Current expert consensus emphasizes that controlling intestinal inflammation often improves peripheral joint symptoms, but axial involvement may require targeted therapy.
Medical professionals recommend that patients maintain detailed symptom logs tracking both digestive and joint symptoms to identify patterns and triggers. This information proves invaluable for treatment optimization and helps distinguish between IBD-related joint pain and other potential causes like medication side effects or unrelated arthritis conditions.
Experts also stress the importance of early intervention, as untreated inflammatory joint disease can lead to permanent joint damage. Regular monitoring and prompt treatment adjustments can prevent long-term complications while maintaining quality of life.
Practical Steps for Managing IBD-Related Joint Pain
- Track symptom patterns: Keep a detailed journal noting when joint pain occurs in relation to digestive symptoms, stress levels, weather changes, and medication timing to identify personal triggers and patterns.
- Communicate comprehensively with your healthcare team: Don’t assume joint symptoms are unrelated to your IBD—discuss all symptoms with your gastroenterologist and ask about referrals to rheumatology if joint pain persists.
- Develop a flexible exercise routine: Focus on low-impact activities that maintain joint mobility without triggering inflammation, and be prepared to modify intensity based on symptom levels.
- Consider anti-inflammatory lifestyle modifications: Implement stress reduction techniques, prioritize sleep hygiene, and explore dietary approaches that may benefit both gut and joint inflammation.
- Stay proactive about treatment adjustments: Work with your healthcare team to optimize medications that address both intestinal and joint inflammation, understanding that this may require specialized therapies or combination approaches.
Moving Forward with Comprehensive IBD Care
The recognition of joint pain as a legitimate and common complication of Crohn’s disease represents an important shift toward more holistic IBD care. Rather than viewing digestive and joint symptoms as separate issues, understanding their connection empowers patients to seek appropriate treatment and develop more effective management strategies.
This knowledge also validates the experiences of countless IBD patients who have struggled with unexplained joint pain, providing both answers and hope for better management. As research continues to unveil the complex relationships between gut inflammation and systemic health, patients can expect more targeted and effective treatment options.
If you’re experiencing joint symptoms alongside your IBD, remember that you’re not alone in this challenge. Share your experiences with our community—your insights might help fellow patients recognize similar patterns in their own health journey.
Source: This post summarizes reporting from WebMD. Read the original article.







