Understanding the Hidden Connection: How IBD Can Affect Your Liver and Bile Ducts
Summary of HCPLive
IBD Movement provides news analysis and insights for the IBD community. Always consult your healthcare provider for personal medical advice.
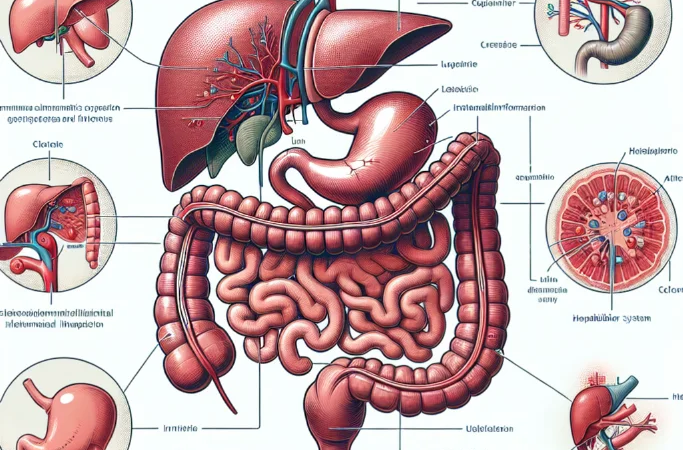
If you’re living with inflammatory bowel disease (IBD), you might think your concerns are limited to your digestive tract. However, a growing body of medical expertise is shedding light on a complex relationship that many people with IBD aren’t aware of: the connection between IBD and hepatobiliary disease, which affects the liver and bile ducts. This emerging understanding could significantly impact how you and your healthcare team approach your overall IBD management and long-term health monitoring.
What Medical Experts Are Revealing About IBD and Liver Health
According to HCPLive, Dr. Natalia Nedelkopoulou has been working to unravel the intricate relationship between IBD and hepatobiliary disease in recent medical discussions. The focus on this connection represents a crucial shift in how healthcare providers are beginning to view IBD as more than just an intestinal condition. As reported by HCPLive, the complexities of managing patients who have both IBD and liver-related complications require specialized understanding and coordinated care approaches.
The medical community is increasingly recognizing that IBD can have far-reaching effects beyond the obvious gastrointestinal symptoms that most patients experience daily. This broader perspective includes understanding how inflammation in the digestive system can potentially impact other organs, particularly the liver and biliary system, which includes the bile ducts and gallbladder.
Healthcare professionals are now paying closer attention to the screening, diagnosis, and management strategies for people with IBD who may also develop hepatobiliary complications. This represents a more comprehensive approach to IBD care that considers the whole person rather than focusing solely on intestinal inflammation.
What This Means for Your IBD Journey
This emerging medical understanding has profound implications for anyone living with IBD. First and foremost, it highlights the importance of viewing your condition through a broader lens. While you may be accustomed to focusing on symptoms like abdominal pain, diarrhea, or fatigue, this research suggests that your healthcare team should also be monitoring your liver function and overall hepatic health as part of your routine IBD care.
The connection between IBD and hepatobiliary disease isn’t entirely surprising when you consider the interconnected nature of your body’s systems. Your liver plays a crucial role in processing medications, including many of the treatments commonly used for IBD management. Additionally, chronic inflammation anywhere in your body can potentially affect other organs, and your liver is particularly susceptible to inflammatory processes.
For people with Crohn’s disease or ulcerative colitis, this information underscores the importance of comprehensive care. You might already be familiar with extraintestinal manifestations of IBD – conditions that affect parts of your body outside your digestive tract, such as joint pain, skin conditions, or eye inflammation. Hepatobiliary complications can be considered another potential extraintestinal manifestation that requires attention.
This evolving understanding also has practical implications for your medication management. Many IBD medications, including immunosuppressants and biologics, require careful monitoring of liver function. If you’re at risk for or already experiencing hepatobiliary complications, your treatment plan may need to be adjusted accordingly. This doesn’t mean your options are limited, but rather that your care team needs to be more strategic in their approach.
The research also suggests that early detection and intervention could be key factors in managing both conditions effectively. This means that routine liver function tests, which you might already be receiving as part of your IBD monitoring, become even more critical. These tests aren’t just checking for medication side effects – they’re also screening for potential complications that could significantly impact your long-term health.
Furthermore, this connection emphasizes the importance of lifestyle factors that support both digestive and liver health. Your diet, alcohol consumption, weight management, and overall wellness practices may have even greater significance when you’re managing both IBD and potential hepatobiliary concerns.
Expert Insights for Patient-Doctor Conversations
Medical experts typically recommend that people with IBD maintain open, ongoing discussions with their healthcare providers about all aspects of their health, not just their digestive symptoms. When it comes to hepatobiliary health, gastroenterologists and hepatologists often work together to provide comprehensive care for patients with both conditions.
You should feel empowered to ask your doctor about liver function monitoring, especially if you’re experiencing symptoms that might be related to hepatobiliary issues, such as unexplained fatigue, abdominal pain in the upper right area, or changes in your skin or eye color. Your healthcare team can help you understand which symptoms warrant immediate attention and which are part of your normal IBD experience.
Practical Steps You Can Take
- Stay current with all recommended blood work and monitoring – liver function tests are particularly important for people with IBD
- Discuss your complete symptom picture with your healthcare team – don’t assume all symptoms are IBD-related without professional evaluation
- Maintain a comprehensive health record that includes both digestive and non-digestive symptoms to help identify patterns
- Ask about coordinated care approaches if you develop hepatobiliary complications – you may benefit from seeing both a gastroenterologist and a hepatologist
- Focus on lifestyle factors that support both digestive and liver health – including nutrition, exercise, and stress management
Looking Forward with Knowledge and Hope
Understanding the connection between IBD and hepatobiliary disease represents progress in comprehensive IBD care. While it might seem overwhelming to consider additional health concerns, this knowledge actually empowers you and your healthcare team to provide more thorough, preventive care. Early awareness and monitoring can lead to better outcomes and more personalized treatment approaches.
This evolving understanding of IBD’s broader impact reinforces the importance of staying engaged with your healthcare team and the IBD community. As research continues to unveil these connections, we’re moving toward more holistic approaches to IBD management that consider your entire health picture, not just your digestive symptoms.
We encourage you to discuss this topic with your healthcare provider and share your experiences with our community. Your insights and questions help all of us better understand and navigate the complexities of living with IBD.
Source: This post summarizes reporting from HCPLive. Read the original article.







