New Imaging Advances Bring Hope for Better Crohn’s Care
If you live with Crohn’s disease, you know that sinking feeling when your doctor orders another scan. Will it show new inflammation? A stricture that needs surgery? Or will it leave you with more questions than answers? The uncertainty can be almost as challenging as the physical symptoms themselves. But here’s something that might lift your spirits: the world of medical imaging is rapidly evolving, and these advances could mean clearer answers and better treatment decisions for all of us in the IBD community.
For too long, many of us have experienced the frustration of inconclusive scans or the anxiety of waiting to understand what’s really happening in our intestines. The good news is that researchers and clinicians are working hard to change that reality.
Summary of MRI, CT, ultrasound, biomarkers help identify Crohn disease strictures
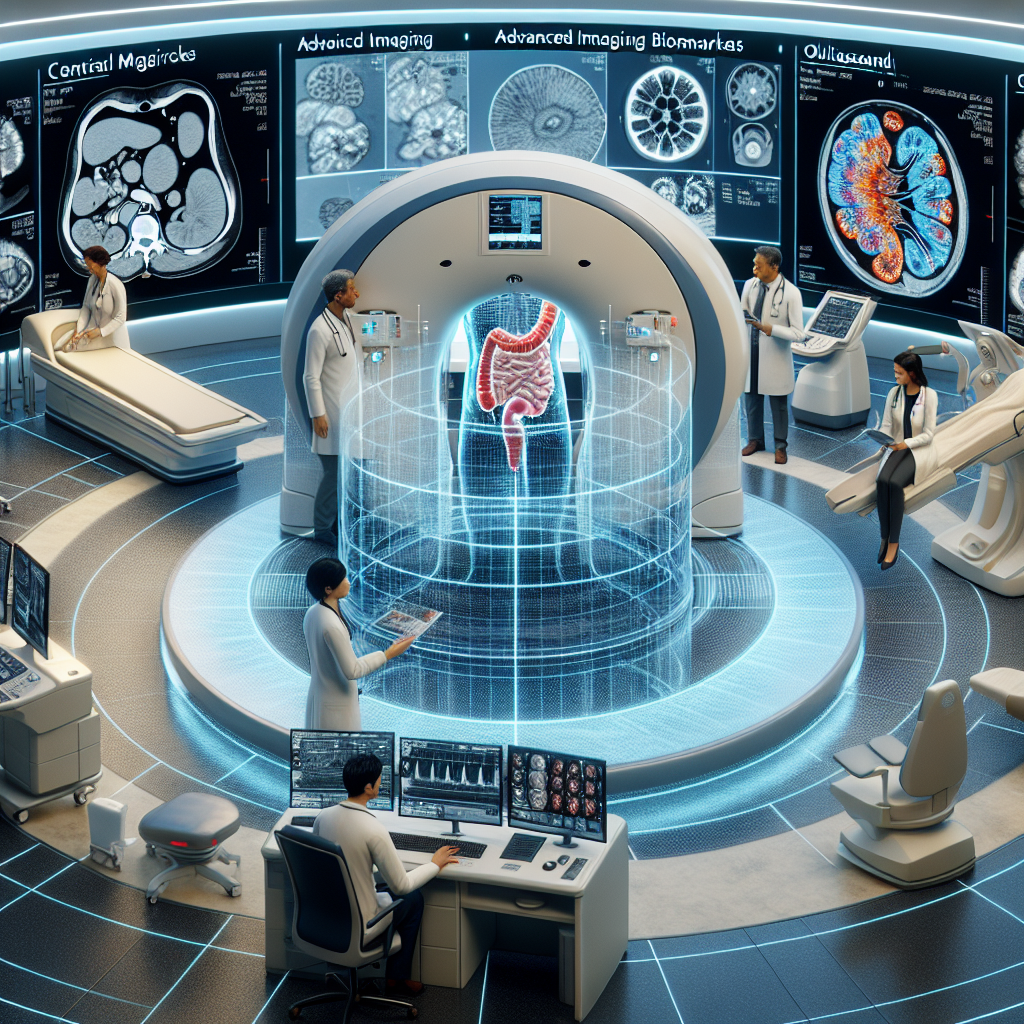
Recent developments in medical imaging are revolutionizing how doctors detect and evaluate strictures—those troublesome narrowings in the intestines that can cause pain, blockages, and so much worry. Traditional imaging methods have sometimes left doctors guessing about whether a stricture is caused by active inflammation (which might respond to medication) or scar tissue (which typically requires surgery).
The breakthrough lies in combining advanced imaging techniques with something called biomarkers—measurable indicators that help predict how strictures will behave. Magnetic Resonance Enterography (MRE) is leading the charge because it doesn’t use radiation and can show both the structure and function of intestinal tissue. This helps doctors distinguish between inflammatory strictures and fibrotic (scarred) ones, which is crucial for choosing the right treatment approach.
CT enterography remains valuable, especially in emergency situations, while ultrasound techniques—including newer methods like contrast-enhanced ultrasound and elastography—offer non-invasive options that can be repeated safely. These imaging biomarkers are helping doctors predict which strictures will respond to medications versus which ones need surgical intervention.
This post summarizes reporting from MRI, CT, ultrasound, biomarkers help identify Crohn disease strictures. Our analysis represents IBD Movement’s perspective and is intended to help patients understand how this news may affect them. Read the original article for complete details.
What This Means for the IBD Community
Let’s talk about what these advances could mean for your day-to-day life with Crohn’s disease. First and foremost, better imaging means fewer surprises. Instead of playing a guessing game about whether your symptoms indicate active inflammation or scar tissue, your medical team will have clearer tools to see what’s actually happening inside your body.
This precision matters enormously for treatment decisions. How many of us have wondered whether we should try another medication or if it’s time to consider surgery? With improved imaging biomarkers, doctors can better predict which strictures are likely to respond to anti-inflammatory medications like biologics, and which ones have progressed to the point where surgical intervention might be the more effective path. This could mean fewer trial-and-error approaches with medications that aren’t likely to work for your specific situation.
From a practical standpoint, the emphasis on non-radiation imaging options like MRE and advanced ultrasound is particularly meaningful for those of us who need frequent monitoring. If you’re someone who’s had multiple CT scans over the years, you’ve probably worried about radiation exposure. The expansion of MRE and ultrasound options means you can get the detailed information your doctor needs without that added concern.
The repeatability factor is huge too. Because ultrasound and MRE don’t carry radiation risks, doctors can use them more liberally to track changes over time. This could lead to earlier detection of problems and more timely adjustments to your treatment plan—potentially preventing some of the complications that arise when strictures progress undetected.
For caregivers and family members, these advances offer something equally valuable: clearer communication from medical teams. When doctors have better data, they can explain your condition and treatment options more clearly. This reduces the anxiety that comes from uncertainty and helps everyone involved make more informed decisions about care.
Questions to Discuss With Your Healthcare Team
These imaging advances present some excellent conversation starters for your next appointment. You might ask your gastroenterologist whether MRE might be appropriate for your monitoring schedule, especially if you’ve been having frequent CT scans. If you’re dealing with symptoms that suggest a possible stricture, inquire about which imaging approach would give the most useful information for your specific situation.
It’s also worth discussing how these newer imaging biomarkers might influence your treatment timeline. If you’re currently on a medication that isn’t providing the relief you hoped for, these advanced imaging techniques might help determine whether it’s worth adjusting your medical therapy or if surgical consultation should be the next step.
Don’t hesitate to ask about the availability of these advanced techniques at your treatment center. Not every facility has the latest MRE capabilities or specialized ultrasound equipment, but knowing what’s available—or where you might need to go for more advanced imaging—can be valuable information for your care planning.
The Bigger Picture for IBD Research
These imaging developments reflect a broader shift toward personalized medicine in IBD care. We’re moving away from the one-size-fits-all approaches that have dominated treatment for decades. Instead, researchers and clinicians are working to match specific treatments to individual disease patterns and characteristics.
The integration of imaging biomarkers with other forms of precision medicine—like genetic testing and advanced blood markers—suggests we’re entering an era where treatment decisions will be based on much more comprehensive data about each person’s unique disease profile. This could significantly improve outcomes while reducing the need for invasive procedures and unsuccessful medication trials.
For the research community, these imaging advances are opening new possibilities for clinical trials. Better ability to measure and monitor strictures means researchers can more accurately assess whether new treatments are working, potentially speeding the development of breakthrough therapies.
The hope is that as these technologies become more widespread and standardized, they’ll become routine parts of IBD care rather than specialized tools available only at major medical centers. This democratization of advanced imaging could help reduce disparities in care quality that currently exist between different regions and healthcare systems.
While we’re still in the early stages of implementing these advances broadly, the trajectory is encouraging. The combination of better imaging technology, artificial intelligence to analyze complex image data, and growing understanding of IBD biology suggests that the next decade could bring dramatic improvements in how we diagnose, monitor, and treat Crohn’s disease.
These advances represent more than just technical improvements—they offer hope for reduced anxiety, more targeted treatments, and ultimately better quality of life for everyone in our community. As these tools become more accessible, we can look forward to a future where the uncertainty that has long characterized IBD care gives way to clearer answers and more confident treatment decisions.
IBD Movement provides information for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.







