Precision Microbiota Therapy: A New Hope for Crohn’s Disease
If you’ve been living with Crohn’s disease for any length of time, you’ve probably felt that familiar frustration—the one that comes when treatments feel like they’re always playing catch-up with your symptoms. Just when you think you’ve found your rhythm, a flare reminds you that your gut has its own unpredictable agenda. But what if the answer isn’t just about managing inflammation or suppressing your immune system? What if it’s about understanding the unique ecosystem living inside your digestive tract?
For many of us in the IBD community, the idea that our gut bacteria might hold the key to better health isn’t entirely new. We’ve heard about probiotics, tried fermented foods, and maybe even wondered if our microbiome is somehow different from people without IBD. Now, emerging research is suggesting that precision microbiota therapy—treatments tailored to your specific bacterial and fungal communities—might offer a more targeted approach to managing Crohn’s disease.
Summary of Read the full article here.
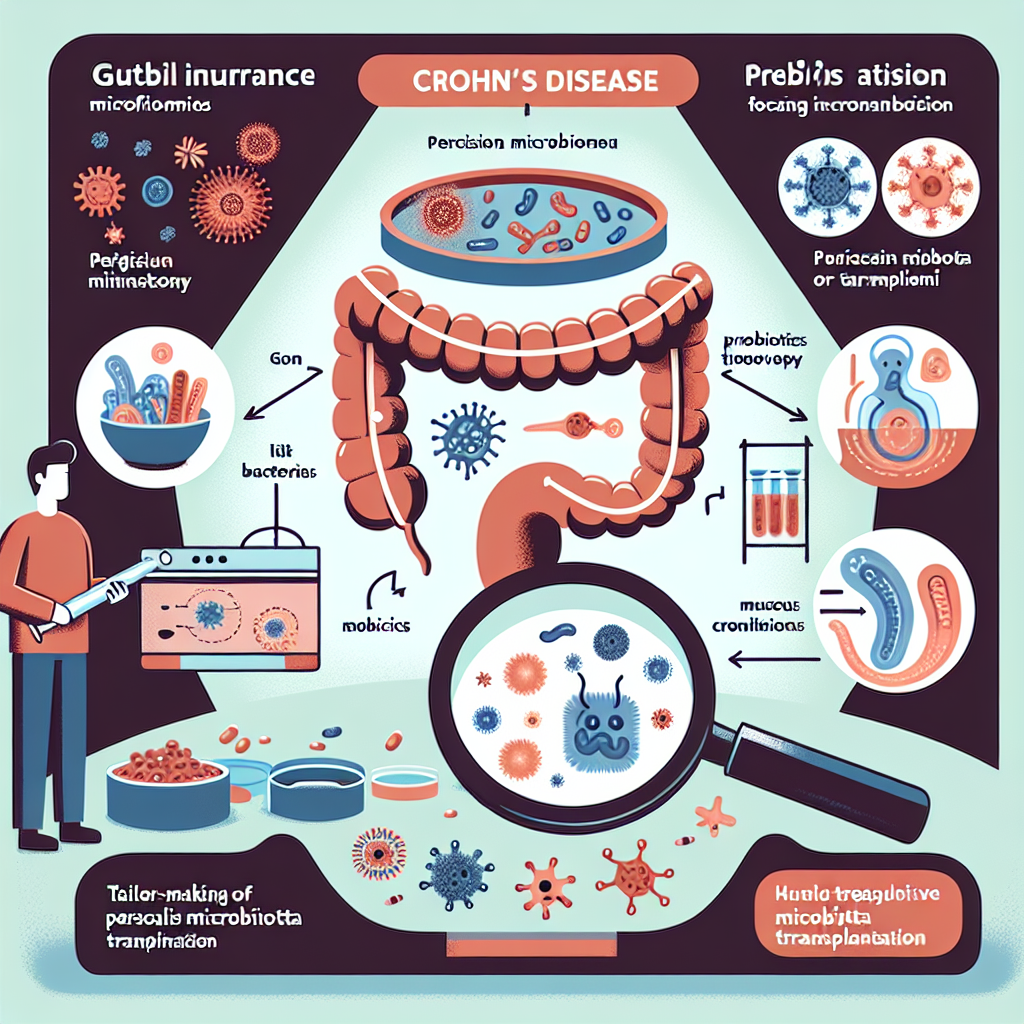
Recent research is exploring how precision microbiota therapy could transform Crohn’s disease treatment by focusing on the specific imbalances in each person’s gut bacteria and fungi. Unlike traditional approaches that use broad treatments, this method involves detailed profiling of an individual’s microbiome to identify exactly which microbes are out of balance. Based on these findings, doctors could prescribe targeted interventions—specific probiotic strains, prebiotic compounds, or even carefully selected fecal microbiota transplants—designed to restore harmony to that person’s unique microbial community.
The therapy aims to go beyond symptom management by addressing what researchers believe may be a root cause of Crohn’s disease: disrupted communication between our gut bacteria and our immune system. By restoring the right balance of microbes, these treatments could potentially reduce inflammation, strengthen the intestinal barrier, and even help prevent future flares. The approach represents a shift from one-size-fits-all treatments to personalized medicine that acknowledges each person’s gut microbiome is as unique as their fingerprint.
This post summarizes reporting from Read the full article here.. Our analysis represents IBD Movement’s perspective and is intended to help patients understand how this news may affect them. Read the original article for complete details.
What This Means for the IBD Community
This development feels particularly significant for those of us who’ve felt like we’re fighting our own bodies every day. The concept of precision microbiota therapy acknowledges something many IBD patients have long suspected: that our individual experiences with Crohn’s disease are deeply personal, and our treatments should be too.
For years, many of us have noticed patterns that don’t quite fit the textbook descriptions of IBD. Maybe certain foods that trigger flares in your friend with Crohn’s don’t affect you at all. Perhaps you’ve had success with a probiotic that did nothing for others in your support group. These aren’t coincidences—they’re likely reflections of the unique microbial communities we each carry.
The practical implications could be transformative. Instead of the traditional trial-and-error approach where patients cycle through different medications hoping to find one that works, precision microbiota therapy could offer a roadmap based on your specific biological markers. This could mean:
- Fewer failed treatment attempts and faster path to effective therapy
- Reduced exposure to medications that might not work for your specific case
- Better understanding of why certain dietary changes help some people but not others
- More targeted probiotic recommendations instead of generic over-the-counter options
But perhaps most importantly, this approach validates something many IBD patients have felt intuitively—that healing involves working with our bodies’ natural systems rather than just suppressing them. The focus on restoring balance rather than simply blocking inflammation represents a fundamental shift in how we think about IBD treatment.
Of course, this isn’t a magic bullet, and we should be realistic about timelines. Precision microbiota therapy is still largely in the research phase, and it will likely be several years before these approaches become widely available in clinical practice. The science of mapping individual microbiomes and translating that data into effective treatments is incredibly complex.
There are also practical questions that many of us are probably already wondering about. Will insurance cover microbiome testing and personalized treatments? How often would someone need to have their microbiome analyzed? What happens if the prescribed microbial interventions don’t take hold or get disrupted by antibiotics or other medications?
Questions to Discuss with Your Healthcare Team
If this research resonates with you, here are some questions you might consider bringing up during your next appointment:
- Are there any clinical trials for precision microbiota therapy that I might be eligible for?
- Should I consider any specific microbiome testing now, or wait for more standardized approaches?
- How might my current medications affect my microbiome, and are there ways to protect it?
- What’s your perspective on targeted probiotics versus broad-spectrum options for someone with my specific IBD profile?
The beauty of this research is that it’s opening up conversations about IBD treatment that go beyond just managing symptoms. It’s encouraging healthcare providers and patients to think about the gut as a complex ecosystem that needs nurturing, not just controlling.
This research also fits into a broader trend we’re seeing in IBD care toward personalized medicine. From genetic testing that helps predict which medications might work best, to dietary approaches that consider individual food sensitivities, the field is moving away from the assumption that all IBD patients should be treated identically. Precision microbiota therapy represents another piece of this personalized puzzle.
For those of us who’ve felt discouraged by the unpredictable nature of Crohn’s disease, this research offers something precious: hope grounded in science. It suggests that the frustrating variability in how we respond to treatments isn’t a bug in the system—it’s a feature that can be leveraged to create more effective, individualized care.
The research also validates many of the instincts IBD patients have developed over years of living with their condition. That gut feeling (literally) about which foods make you feel better, or the sense that your body needs something different from what worked for other people—these intuitions might have solid biological backing.
While we wait for precision microbiota therapy to become more widely available, there are ways we can start thinking about our gut health more strategically. This might include keeping detailed food and symptom diaries, paying attention to how different stressors affect our digestion, or working with healthcare providers who are interested in the role of the microbiome in IBD.
The shift toward precision microbiota therapy represents more than just another treatment option—it’s a recognition that healing IBD might require understanding and working with the incredible complexity of our individual biology. For a community that’s often felt like their bodies were working against them, this approach offers the possibility of treatments that work with our natural systems instead.
This research reminds us that we’re not just patients with a disease—we’re individuals with unique biological signatures that might hold the keys to our own healing. That’s not just scientifically exciting; it’s deeply empowering for anyone who’s ever felt like their IBD was something happening to them rather than something they could actively address.
While precision microbiota therapy is still emerging, it represents exactly the kind of innovative thinking our community needs. It acknowledges the complexity of IBD while offering concrete hope for more effective treatments. Most importantly, it recognizes that each person’s journey with Crohn’s disease is unique—and their treatment should be too.
IBD Movement provides information for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.







