After Surgery, IBD Can Still Surprise Us: A Facial Wound’s Message
If you’ve had major IBD surgery—especially a total colectomy—you might think the worst is behind you. Many of us cling to the hope that removing the diseased bowel means we can finally put IBD in the rearview mirror. But sometimes, our bodies have other plans, and IBD finds ways to remind us it’s still part of our story.
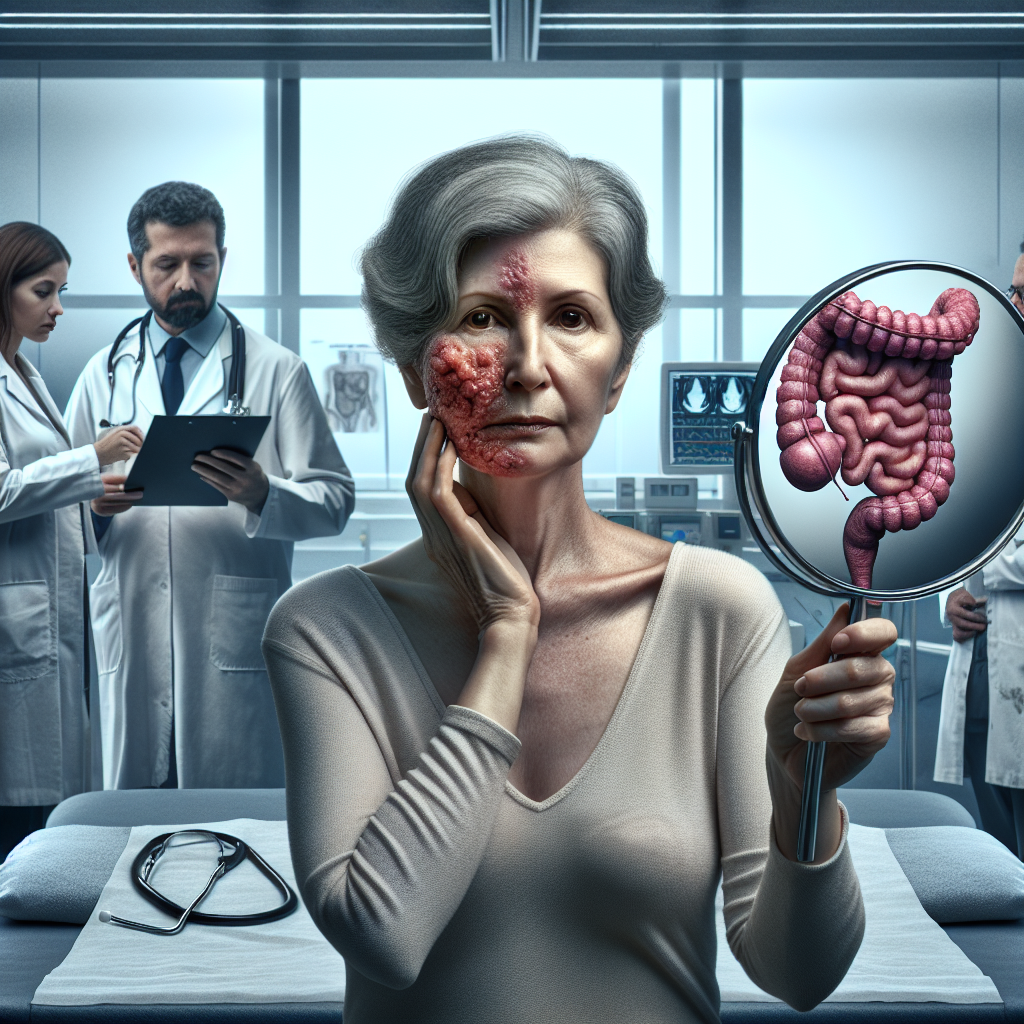
A recent case report tells the story of a woman who thought she’d beaten ulcerative colitis with surgery, only to discover that IBD was quietly waiting in the wings, ready to make an unexpected appearance on her face of all places.
Summary of Cureus
Researchers recently published a case study about a middle-aged woman who had undergone a total colectomy (complete removal of her colon) for ulcerative colitis and was considered to be in remission. Years later, she developed a rapidly growing, painful ulcer on the right side of her face that initially looked like it might be an infection or injury.
After thorough testing, doctors discovered this wasn’t an ordinary wound—it was pyoderma gangrenosum, a rare but serious skin condition that creates deep, painful ulcers. What made this case particularly striking was the location: pyoderma gangrenosum typically appears on the legs, but this patient developed it on her face, which is extremely uncommon.
The most important finding was that this skin condition revealed her IBD was still active in her system, despite having no intestinal symptoms and no colon. The doctors treated her with steroids and immune-suppressing medications, which helped heal the facial wound and improved her overall health.
This post summarizes reporting from Cureus. Our analysis represents IBD Movement’s perspective and is intended to help patients understand how this news may affect them. Read the original article for complete details.
What This Means for the IBD Community
This case hits close to home for many of us in the IBD community, especially those who’ve undergone major surgery or are considering it. Let’s break down what this really means for our daily lives and long-term health journey.
Surgery Isn’t Always the Final Answer
Many of us view colectomy as the ultimate solution—remove the diseased organ, remove the problem. This case reminds us that IBD is a systemic condition, meaning it affects our entire body’s immune system, not just our intestines. Even after removing the colon, the underlying inflammatory process that drives IBD can continue to affect other parts of our body.
For those considering surgery or who’ve already had it, this doesn’t mean surgery was wrong or ineffective. Colectomy saves lives and dramatically improves quality of life for many patients. Rather, it means we need to maintain realistic expectations and stay vigilant about our overall health.
Extra-Intestinal Manifestations Are Real and Unpredictable
About 25-40% of people with IBD experience symptoms outside their digestive system—what doctors call extra-intestinal manifestations. These can include joint pain, eye problems, liver issues, and skin conditions like pyoderma gangrenosum. This case shows us that these manifestations can appear even when our intestinal symptoms seem under control.
What’s particularly unsettling about this case is how unexpected the presentation was. Facial pyoderma gangrenosum is extremely rare, which means even experienced doctors might not immediately recognize it. This highlights the importance of advocating for ourselves and seeking second opinions when something doesn’t feel right, especially if we have a history of IBD.
The Emotional Impact of Unexpected Flares
Imagine thinking you’ve conquered IBD through surgery, only to have a painful, disfiguring wound appear on your face. The psychological impact of such an experience can be devastating. It challenges our sense of control and our belief in our recovery narrative.
This case reminds us that healing from chronic illness is rarely linear. We might have periods of feeling completely normal, followed by unexpected challenges that test our resilience. Having a strong support system and mental health resources becomes crucial for navigating these unpredictable moments.
Questions to Discuss with Your Healthcare Team
If you’ve had IBD surgery or are in remission, consider discussing these questions with your doctor:
- What extra-intestinal manifestations should I watch for, given my specific IBD history?
- How often should I have follow-up appointments and monitoring, even if I feel well?
- What unusual symptoms should prompt me to seek immediate medical attention?
- Should I inform other healthcare providers (dermatologists, eye doctors, etc.) about my IBD history?
- What’s my personal risk level for developing conditions like pyoderma gangrenosum?
The Importance of Comprehensive IBD Care
This case reinforces why comprehensive IBD care involves more than just gastroenterology. The most effective treatment approach often includes dermatologists, rheumatologists, ophthalmologists, and mental health professionals who understand the systemic nature of IBD.
Many IBD centers now offer multidisciplinary clinics where you can see multiple specialists in one visit. If you don’t have access to such a center, make sure your various healthcare providers communicate with each other about your IBD history.
Looking at the Bigger Picture
While this case might initially seem frightening, it actually represents progress in IBD understanding and treatment. The fact that doctors could quickly diagnose and effectively treat this rare presentation shows how far we’ve come in recognizing the systemic nature of IBD.
The patient in this case responded well to treatment with steroids and immunosuppressive medications. This suggests that even when IBD surprises us with unusual presentations, we have effective tools to fight back. The key is rapid recognition and appropriate treatment.
Moreover, cases like this help educate the medical community about rare presentations of IBD, potentially leading to faster diagnosis and treatment for future patients who might experience similar symptoms.
The bottom line is that this case, while concerning, also demonstrates the resilience of the human body and the effectiveness of modern IBD treatments when properly applied. It reminds us that our IBD journey continues throughout our lives, but we have the knowledge, tools, and support systems to handle whatever comes our way.
Remember, knowledge is power in managing IBD. The more we understand about the potential complexities of our condition, the better equipped we are to recognize problems early and advocate for appropriate care. This case study, while highlighting an unusual scenario, ultimately empowers us with information that could prove valuable in our own health journey.
IBD Movement provides information for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.







