When Crohn’s Strikes Your Bladder: A Rare but Real Reality
You thought you had mapped every twist and turn of living with Crohn’s disease. The bathroom urgency, the careful food choices, the way inflammation seems to dictate your schedule—these have become part of your daily navigation. But then your body starts sending signals from somewhere unexpected, and suddenly even your experienced gastroenterologist is scratching their head.
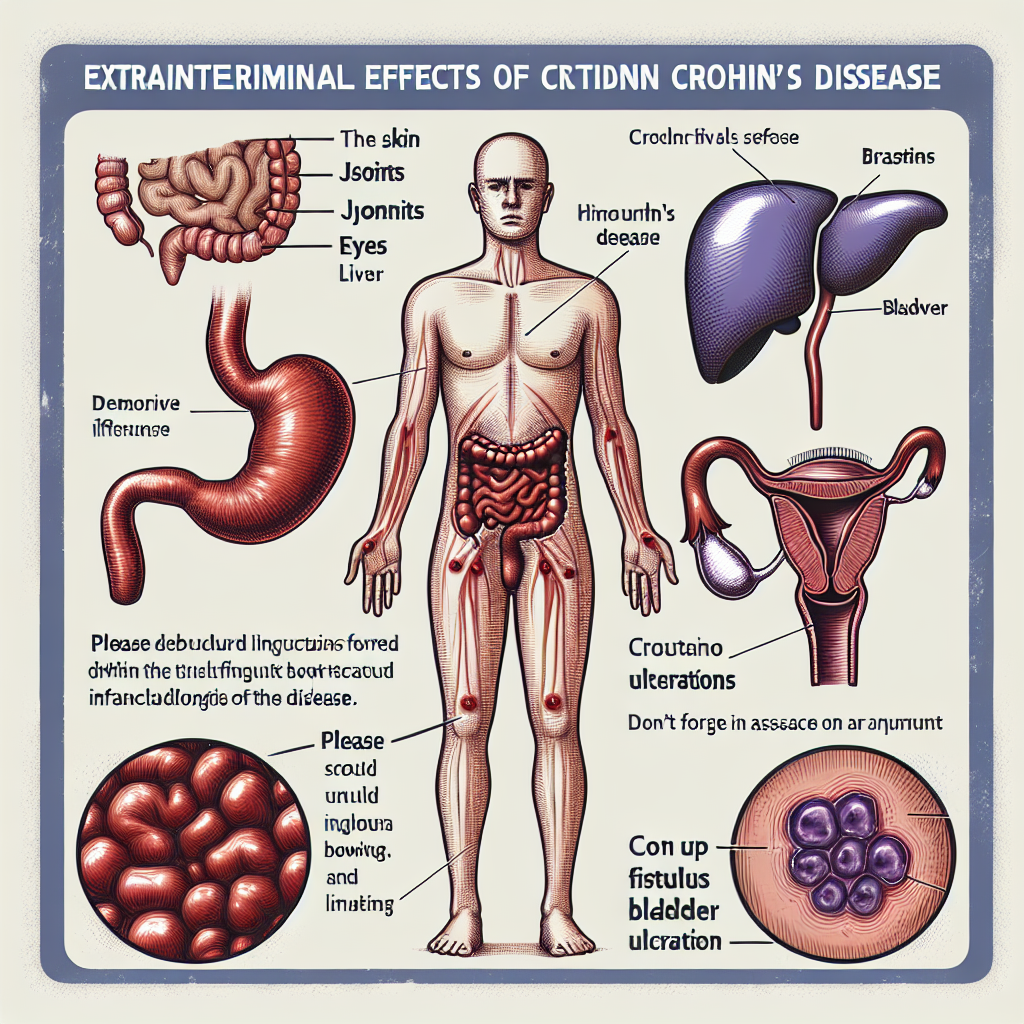
What if I told you that Crohn’s inflammation doesn’t always stay within the neat boundaries of your digestive system? Sometimes, this unpredictable disease ventures into territory that catches everyone off guard—including places like your bladder.
Summary of here
Medical researchers have documented a rare but important manifestation of Crohn’s disease called non-fistulous bladder ulceration. Unlike the more commonly recognized bladder complications that occur when a fistula (abnormal connection) forms between the intestine and urinary tract, this condition involves direct inflammatory damage to the bladder itself.
When this happens, patients may experience symptoms like bladder pain, frequent urination, or blood in their urine—symptoms that can easily be mistaken for a urinary tract infection or other urological problems. The challenge is that many healthcare providers, even those familiar with Crohn’s disease, don’t immediately consider that the inflammation could be directly affecting the bladder without an obvious intestinal connection.
This can lead to delayed diagnosis and inappropriate treatments, as doctors may focus on treating presumed infections or looking for fistulas that don’t actually exist. The key insight from this research is that Crohn’s disease can cause bladder ulcers through direct inflammatory processes, expanding our understanding of how this systemic condition can manifest throughout the body.
This post summarizes reporting from here. Our analysis represents IBD Movement’s perspective and is intended to help patients understand how this news may affect them. Read the original article for complete details.
What This Means for the IBD Community
This research highlights something many of us in the IBD community know all too well: Crohn’s disease is a master of disguise. Just when you think you understand its patterns, it finds new ways to remind you that it’s a systemic inflammatory condition, not just a digestive disorder.
For those of us living with Crohn’s, this information is both unsettling and empowering. It’s unsettling because it adds another item to our already lengthy list of potential complications. But it’s empowering because knowledge is our greatest weapon against misdiagnosis and delayed treatment.
From a practical standpoint, this research suggests we need to be more vigilant about urinary symptoms that don’t respond to typical treatments. If you’re experiencing persistent bladder pain, frequent urination that seems different from your usual patterns, or blood in your urine, these symptoms deserve serious attention—especially if they’re not responding to standard urinary tract infection treatments.
This also underscores the importance of having a healthcare team that thinks beyond the obvious. While most doctors correctly look for fistulas when Crohn’s patients develop urinary symptoms, this research reminds us that direct bladder inflammation is also possible. Your gastroenterologist and urologist need to work together, considering all possibilities rather than just the most common ones.
One particularly important implication is for symptom tracking. Many of us already keep detailed logs of our digestive symptoms, but this research suggests we should also be noting urinary changes. Patterns matter, and sometimes what seems like a simple UTI might actually be your Crohn’s inflammation extending its reach.
This finding also speaks to the broader challenge of living with a rare manifestation of an already complex disease. When you’re dealing with something that even specialists find unusual, you often become your own best advocate. This research gives us language and evidence to bring to our healthcare providers when we’re experiencing symptoms that don’t fit the typical Crohn’s playbook.
For caregivers and family members, this information is equally important. Understanding that Crohn’s can manifest in unexpected ways helps create a support system that takes all symptoms seriously, even when they seem unrelated to the “typical” disease presentation.
The research also raises important questions worth discussing with your healthcare team: Should routine urinalysis be part of standard Crohn’s monitoring? How quickly should persistent urinary symptoms be escalated for specialist evaluation? What imaging or testing might be helpful when urinary symptoms don’t respond to standard treatments?
Perhaps most importantly, this research reinforces that our bodies are interconnected systems. The inflammation that drives Crohn’s disease doesn’t respect the neat anatomical boundaries we draw in textbooks. This systemic nature of the disease is why comprehensive, coordinated care is so crucial.
This finding fits into a broader trend in IBD research toward understanding extraintestinal manifestations—the ways inflammatory bowel disease affects organs and systems beyond the digestive tract. As we learn more about these connections, we’re better equipped to provide comprehensive care that addresses the whole person, not just the primary disease site.
For many in our community, this research will resonate with their own experiences of mysterious symptoms that took time to connect back to their Crohn’s disease. It validates the frustrating journey many face when symptoms don’t fit neat diagnostic categories, and it provides hope that continued research will uncover more of these hidden connections.
The key takeaway isn’t to become anxious about every new symptom, but rather to maintain open communication with your healthcare team about any persistent or unusual symptoms. Your lived experience with your body, combined with your medical team’s expertise, creates the best foundation for catching these rare manifestations early.
While bladder involvement in Crohn’s disease remains uncommon, being aware of this possibility ensures that if you do experience persistent urinary symptoms, you and your healthcare team can consider all potential causes. This knowledge transforms you from a passive patient into an informed advocate for your own comprehensive care.
Early recognition and appropriate treatment of any Crohn’s-related complications, including rare ones like non-fistulous bladder ulceration, can prevent more serious problems down the road. This research gives us another piece of the puzzle in understanding how to live well with this complex condition.
The bottom line is that Crohn’s disease continues to teach us about the interconnected nature of our bodies. While we can’t predict every twist this condition might take, staying informed about possibilities like bladder involvement helps us partner more effectively with our healthcare teams. Knowledge doesn’t eliminate uncertainty, but it does give us tools to navigate it more confidently.
This research reminds us that advocating for comprehensive care isn’t just about getting the best treatment for our known symptoms—it’s about ensuring our healthcare teams consider the full spectrum of ways our condition might manifest. In a healthcare system that often focuses on single-organ specialties, this kind of systems thinking becomes crucial for those of us living with complex, multi-system conditions.
IBD Movement provides information for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.







