When Skin Wounds Signal Hidden IBD: A First Warning Sign
Picture this: you notice a painful, unusual wound on your skin that doesn’t heal like it should. You try the usual remedies, visit your doctor, maybe even see a dermatologist. But nothing seems to work, and the wound keeps getting worse. What you might not realize is that this stubborn skin problem could be your body’s way of telling you something important is happening with your immune system—possibly even before you experience any digestive symptoms.
For those of us in the IBD community, we know that our condition doesn’t always stay neatly contained to our digestive tract. Sometimes, the first signs of inflammatory bowel disease show up in the most unexpected places, including our skin. Understanding these connections can be crucial for early detection and treatment.
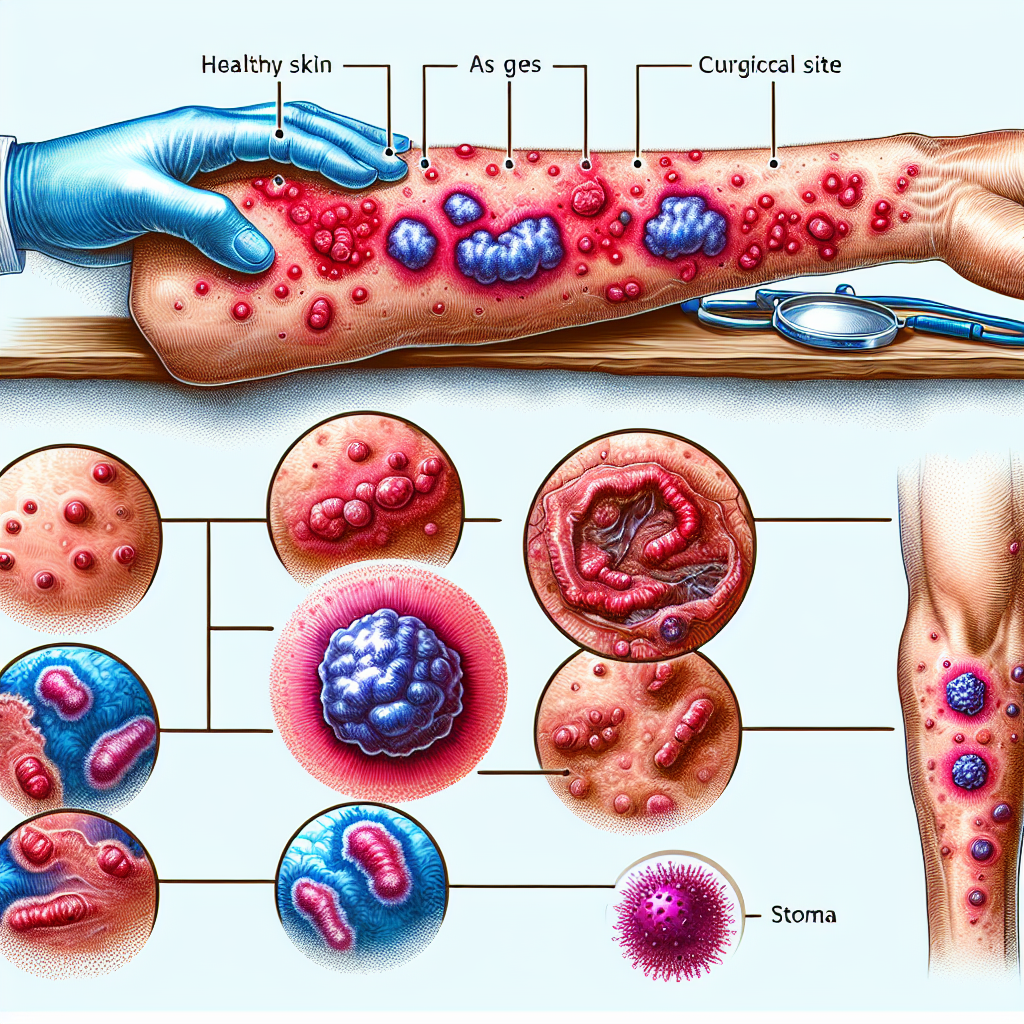
Sometimes, those painful, purple-edged ulcers that seem to appear out of nowhere—especially if they spread fast and don’t respond to normal treatments—are actually your immune system waving a red flag before classic gut trouble even starts. Pyoderma gangrenosum can be so much more than “just” a skin problem; it can be the first warning sign of inflammatory bowel disease, showing up even before the usual stomach pain, diarrhea, or weight loss. These persistent sores that won’t heal can be critical clues, and catching these skin changes early might lead to life-changing answers and timely diagnosis.
What This Means for the IBD Community
This connection between skin manifestations and IBD is more significant than many people realize, and it carries important implications for all of us who live with or care for someone with inflammatory bowel disease. Understanding this relationship can be truly life-changing for several reasons.
First, let’s talk about early detection. Many IBD patients spend months or even years seeking answers for their digestive symptoms. The average time to diagnosis can be frustratingly long, during which inflammation continues to damage the intestines. But when pyoderma gangrenosum appears first, it could potentially fast-track the diagnostic process. Healthcare providers who recognize this skin condition’s association with IBD might order the appropriate tests sooner, leading to earlier treatment and better long-term outcomes.
For family members of IBD patients, this information is particularly valuable. IBD has genetic components, and family members are at higher risk of developing the condition. If someone in an IBD family develops these characteristic skin wounds, it might prompt earlier screening and monitoring for digestive symptoms.
This also highlights the importance of looking at our bodies as interconnected systems rather than isolated parts. IBD is a systemic inflammatory condition, and pyoderma gangrenosum is just one example of how inflammation can manifest beyond the digestive tract. Other extraintestinal manifestations include joint pain, eye inflammation, and liver problems. Recognizing these patterns helps both patients and healthcare providers take a more comprehensive approach to treatment.
From a practical standpoint, if you’re experiencing unusual skin wounds alongside any digestive concerns—even mild ones you might have dismissed—it’s worth discussing both symptoms together with your healthcare provider. The combination could provide important diagnostic clues that might not be apparent when considering each symptom in isolation.
Questions to Discuss with Your Healthcare Team
If you or a loved one is dealing with persistent, unusual skin wounds, especially those with the characteristics of pyoderma gangrenosum, consider discussing these questions with your healthcare provider:
- Could these skin symptoms be related to an underlying inflammatory condition like IBD?
- What tests might help determine if there’s a connection between my skin symptoms and digestive health?
- Should I be monitoring for any specific digestive symptoms, given these skin changes?
- If I have a family history of IBD, does this skin condition change my risk profile?
- What’s the best approach to treating both the skin symptoms and any potential underlying inflammation?
The Broader Picture: Systemic Inflammation and IBD
This connection between skin manifestations and IBD reflects a broader understanding that’s been evolving in the medical community: inflammatory bowel disease is truly a systemic condition. While the primary inflammation occurs in the digestive tract, the immune dysfunction that drives IBD can affect multiple organ systems.
This systemic nature of IBD explains why many of us experience symptoms beyond digestive issues. Joint pain affects up to 40% of IBD patients. Eye inflammation, skin problems, and even increased risk of certain cancers are all part of the broader IBD picture. Understanding this helps explain why comprehensive, multidisciplinary care is so important for IBD management.
For healthcare providers, this reinforces the importance of considering IBD in patients presenting with certain extraintestinal manifestations, even in the absence of obvious digestive symptoms. For patients, it emphasizes the value of comprehensive health monitoring and the importance of mentioning seemingly unrelated symptoms to your IBD care team.
Hope and Empowerment Through Knowledge
While it might seem overwhelming to think about all the ways IBD can affect our bodies, knowledge is ultimately empowering. Understanding these connections means we can be better advocates for ourselves and our loved ones. It means we can recognize warning signs earlier and seek appropriate care sooner.
The relationship between pyoderma gangrenosum and IBD also represents the kind of medical insight that comes from treating patients as whole people rather than collections of separate symptoms. This holistic approach to healthcare is becoming increasingly important in managing complex conditions like IBD.
For those who might be experiencing unexplained skin wounds along with any digestive concerns, don’t hesitate to mention both to your healthcare provider. Sometimes it’s the combination of symptoms, rather than any single symptom, that provides the key to diagnosis and effective treatment.
The connection between mysterious skin wounds and IBD reminds us that our bodies are constantly communicating with us. When we learn to listen—and when we have healthcare providers who understand these complex relationships—we’re better equipped to maintain our health and catch problems early. While pyoderma gangrenosum can be a challenging condition to deal with, recognizing its potential connection to IBD could be the key to getting comprehensive treatment and improving long-term health outcomes. Knowledge truly is power, especially when it comes to managing complex inflammatory conditions like IBD.
IBD Movement provides information for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.







