Beyond ‘Just Stress’: Understanding the Real Impact of Crohn’s
That gnawing feeling in your stomach isn’t going away with deep breathing exercises. The exhaustion isn’t something a good night’s sleep can fix. And the pain—that deep, gripping pain—defies every stress management technique you’ve tried. If you’re living with Crohn’s disease, you know that dismissive phrase all too well: “It’s probably just stress.” But you also know it’s so much more than that.
Living with Crohn’s means carrying an invisible burden that others can’t see or fully understand. It’s waking up each morning wondering if today will be a “good day” or if you’ll spend it managing symptoms that can derail even the best-laid plans. It’s the constant mental calculation of bathroom locations, meal timing, and energy reserves—a complex dance that becomes second nature but never gets easier.
Summary of here
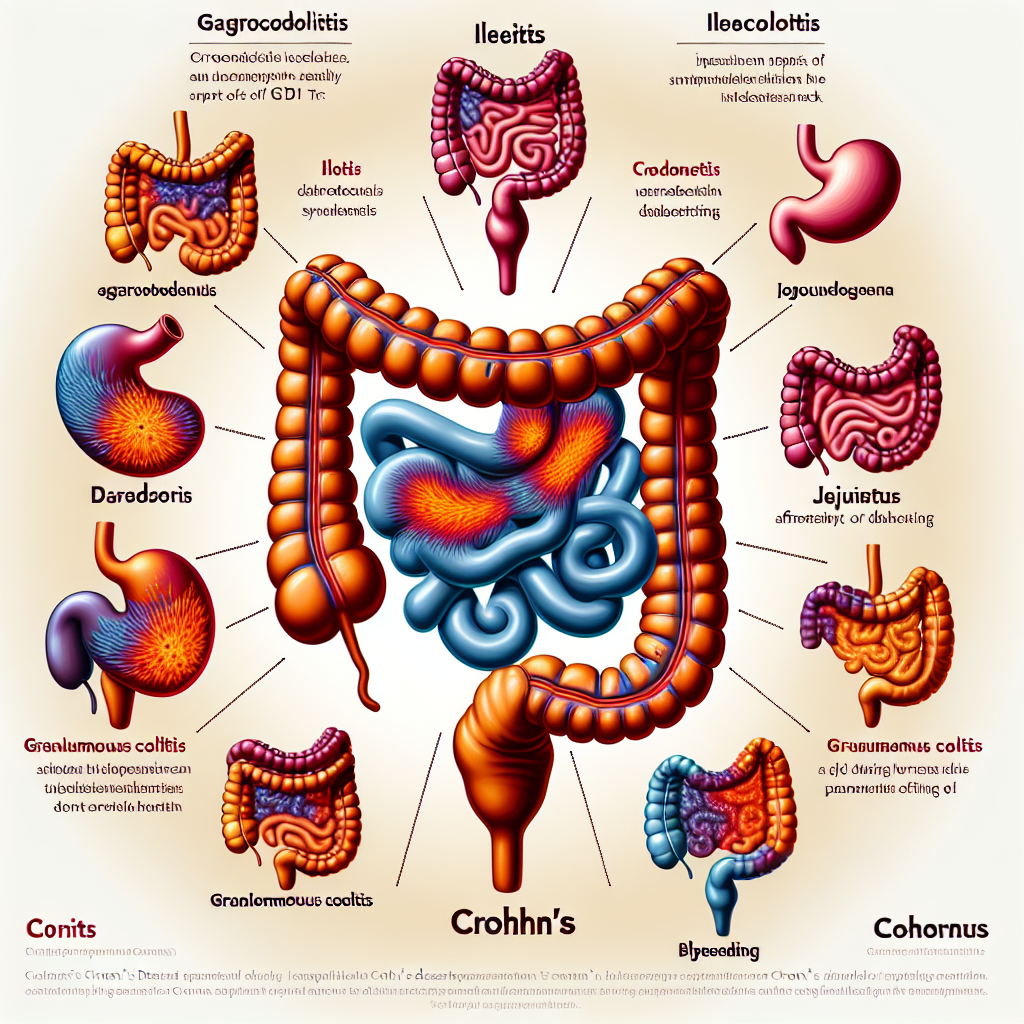
Crohn’s disease is a chronic inflammatory condition that affects the digestive tract, but its impact extends far beyond stomach troubles. Unlike surface-level digestive issues, Crohn’s inflammation penetrates through the entire thickness of the bowel wall, creating deep and lasting effects throughout the body. The condition can strike anywhere from the mouth to the anus, with symptoms that include unpredictable abdominal pain, urgent diarrhea, severe fatigue, weight loss, and loss of appetite.
What makes Crohn’s particularly challenging is its unpredictable nature—symptoms can flare up suddenly and then disappear just as quickly, creating a cycle of uncertainty and anxiety. The inflammation doesn’t stay contained to the digestive system either; it can manifest as joint pain, skin rashes, and other systemic symptoms that make it feel like the entire body is under attack.
Different types of Crohn’s affect different parts of the digestive tract—whether the colon, small intestine, or even the stomach—and understanding these distinctions is crucial for developing targeted treatment approaches. Early recognition of symptoms and proper diagnosis opens the door to more effective management strategies and the possibility of reclaiming quality of life.
This post summarizes reporting from here. Our analysis represents IBD Movement’s perspective and is intended to help patients understand how this news may affect them. Read the original article for complete details.
What This Means for the IBD Community
This comprehensive overview of Crohn’s disease validates what many in our community have experienced firsthand: the frustration of having symptoms minimized or misunderstood. When healthcare discussions acknowledge that Crohn’s inflammation affects the entire bowel wall thickness, it reinforces why our symptoms are so much more complex and persistent than simple digestive upset.
For newly diagnosed patients, understanding that Crohn’s can affect different parts of the digestive tract helps explain why experiences vary so widely within our community. Someone with colonic Crohn’s may have different symptoms and treatment responses than someone with small bowel disease. This isn’t about one person’s Crohn’s being “worse” than another’s—it’s about recognizing that this condition manifests uniquely in each person.
The emphasis on targeted care based on disease location and type is particularly encouraging. It suggests that the one-size-fits-all approach to IBD treatment is evolving toward more personalized medicine. This could mean fewer trial-and-error periods with medications that don’t match your specific disease pattern, and more direct paths to effective treatment.
Practical Implications for Daily Life
Understanding the full-thickness nature of Crohn’s inflammation helps explain why healing takes time and why some symptoms persist even when others improve. This knowledge can help you set realistic expectations for treatment timelines and recovery periods. It’s not that you’re “not trying hard enough” to get better—it’s that your body is healing damage that goes deep.
The unpredictable flare pattern described in the overview resonates with the lived experience of planning around uncertainty. Knowing that this unpredictability is a recognized feature of Crohn’s disease can be oddly comforting—it validates the challenge of living with a condition that doesn’t follow a predictable schedule.
For caregivers and family members reading this, the systemic nature of Crohn’s symptoms—including joint pain, skin issues, and fatigue—helps explain why your loved one might struggle with symptoms that seem unrelated to their “stomach condition.” Crohn’s is truly a whole-body disease, and support needs to address this reality.
Questions to Discuss with Your Healthcare Team
This overview raises important questions you might want to explore with your doctor: What type of Crohn’s do you have, and how does that influence your treatment plan? Are there specific monitoring strategies that make sense for your disease location? How can you work together to identify early signs of flares before they become severe?
If you’re experiencing symptoms that extend beyond digestive issues—like joint pain or skin problems—this is validation to bring these concerns to your gastroenterologist. They’re not separate issues to compartmentalize; they’re part of your Crohn’s disease picture.
Connection to Broader IBD Trends
The focus on understanding different Crohn’s presentations aligns with the broader movement toward precision medicine in IBD care. We’re seeing increased research into biomarkers, genetic factors, and personalized treatment approaches that move beyond the traditional step-therapy model.
This comprehensive view of Crohn’s also supports the growing recognition that IBD care needs to be multidisciplinary. Managing a condition that can affect everything from your joints to your skin to your mental health requires a team approach that goes beyond gastroenterology alone.
The emphasis on early diagnosis and targeted care reflects what many advocacy organizations, including those in our community, have been pushing for: faster access to appropriate treatment and reduced time to effective management strategies.
Despite the challenges Crohn’s disease presents, there’s genuine reason for hope in this comprehensive understanding of the condition. When we acknowledge the full scope of what we’re dealing with—the deep inflammation, the systemic effects, the unpredictable patterns—we create space for more effective, compassionate care. You’re not imagining the complexity of your symptoms, and you’re not weak for struggling with a condition that affects your entire body.
The path forward isn’t just about enduring Crohn’s disease; it’s about understanding it well enough to partner effectively with your healthcare team, advocate for your needs, and find moments of genuine wellness within the journey. Every step toward better understanding is a step toward reclaiming parts of your life that Crohn’s may have temporarily taken away.
IBD Movement provides information for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.







