Your Sleep Might Be Warning You About IBD Flares Before You Know It
Have you ever noticed your sleep getting restless or strange right before a flare hits? Maybe you’ve been tossing and turning more, or even acting out your dreams in ways that left you confused and exhausted. For so long, many of us in the IBD community have focused on the obvious warning signs—stomach pain, urgency, that familiar fatigue. But what if our bodies are trying to tell us something important through our sleep patterns, sending us signals we haven’t learned to recognize yet?
This connection between sleep disruption and IBD activity is more profound than many of us realized, and it’s opening up new ways to think about managing our condition proactively.
Summary of here
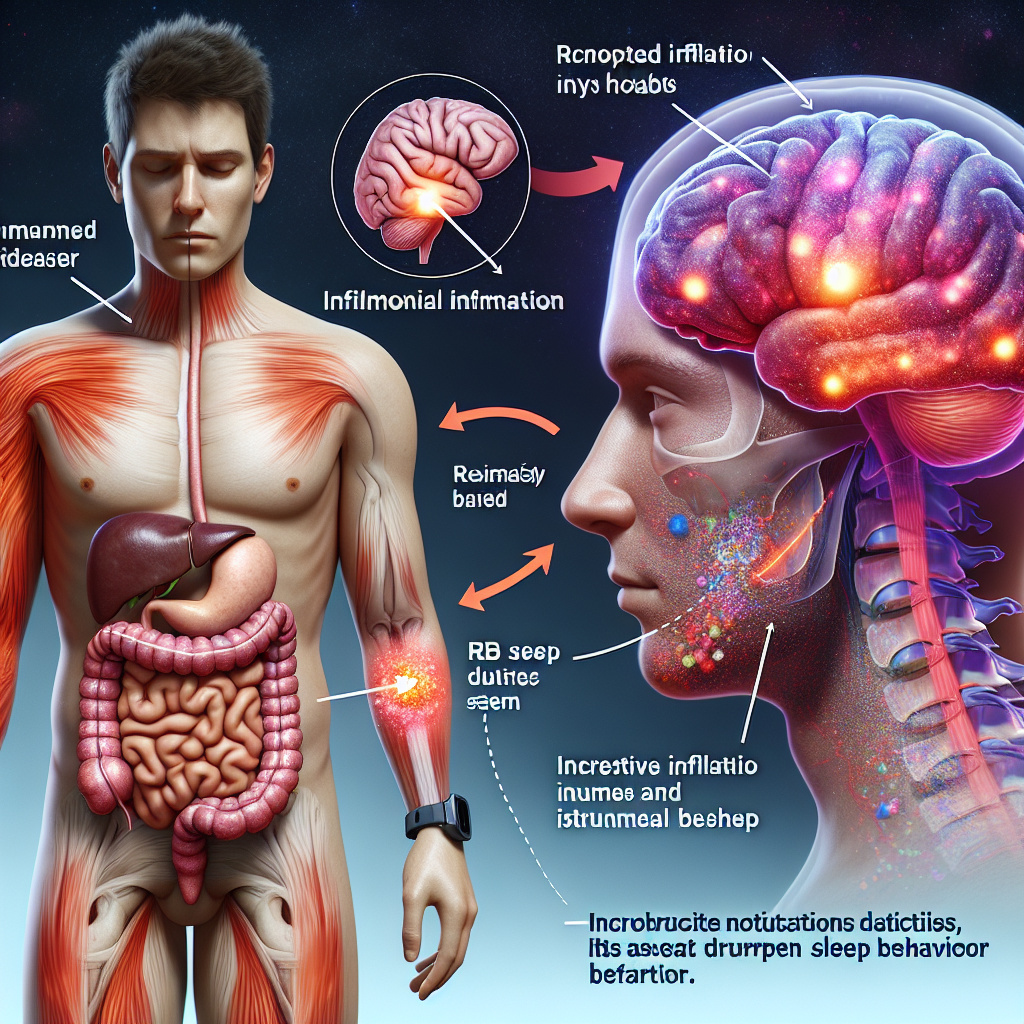
Recent research has uncovered a surprising link between inflammatory bowel disease and sleep disorders, particularly REM sleep behavior disorder (RBD). This condition, where people physically act out their dreams—sometimes violently—was previously thought to mainly affect people with neurological conditions like Parkinson’s disease.
However, scientists are now finding that people with Crohn’s disease and ulcerative colitis are experiencing RBD too, even without signs of neurodegeneration. Using long-term sleep monitoring devices, researchers tracked both gut and brain health simultaneously. What they discovered was remarkable: disrupted sleep patterns often appear before IBD flare-ups occur and can persist even after symptoms improve.
The study suggests that inflammation in the gut doesn’t just affect digestion—it can directly impact the brain’s sleep centers, disrupting the restorative REM sleep that’s crucial for our overall health. This creates a cycle where poor sleep may contribute to more inflammation, which then further disrupts sleep quality.
This post summarizes reporting from here. Our analysis represents IBD Movement’s perspective and is intended to help patients understand how this news may affect them. Read the original article for complete details.
What This Means for the IBD Community
This research fundamentally changes how we might think about monitoring our IBD. Instead of only watching for digestive symptoms, we now have potential justification for paying closer attention to our sleep patterns as an early warning system.
For those of us living with Crohn’s or ulcerative colitis, this could be a game-changer in several ways:
Early Detection Opportunities: If sleep disruption really does precede flare-ups, tracking our sleep quality could give us a head start on treatment. Instead of waiting until pain and urgency hit, we might be able to catch inflammation in its earliest stages. This could mean starting anti-inflammatory treatments sooner, potentially preventing full-blown flares or at least reducing their severity.
A New Symptom to Discuss: Many of us have experienced vivid dreams, restless nights, or even sleepwalking during stressful periods or around flares, but we may not have connected these experiences to our IBD. Now we have scientific backing to bring these concerns to our gastroenterologists. Sleep disturbances aren’t just “something extra” to deal with—they’re potentially a direct manifestation of our inflammatory disease.
Holistic Treatment Approaches: This research supports what many in the IBD community have long suspected: our condition affects our entire body, not just our digestive system. Understanding the gut-brain-sleep connection might lead to more comprehensive treatment plans that address sleep hygiene alongside traditional IBD medications.
Questions to Consider for Your Next Appointment:
- Should I be tracking my sleep patterns along with my digestive symptoms?
- What sleep changes should I report as potentially IBD-related?
- Could addressing my sleep issues help with my overall inflammation levels?
- Are there safe sleep aids that won’t interfere with my IBD medications?
- Should I consider a sleep study if I’m having unusual dream behaviors?
The Bigger Picture: This research fits into a growing understanding of IBD as a systemic inflammatory condition. We’re learning that the inflammation in our guts can affect our joints, skin, eyes, and now clearly our sleep. This validates what many of us have experienced—that IBD isn’t just a “stomach problem” but a whole-body condition that requires whole-body awareness.
The connection also highlights the importance of stress management and mental health support in IBD care. Poor sleep affects our stress levels, which can trigger flares, creating a vicious cycle. Breaking this cycle might require addressing multiple factors simultaneously.
Practical Next Steps: Consider keeping a simple sleep journal alongside your regular symptom tracking. Note not just how many hours you sleep, but how restful it feels, any unusual dreams or movements, and how your sleep quality correlates with your IBD symptoms. Many smartphone apps can help track sleep patterns automatically.
This isn’t about adding another thing to worry about—it’s about gaining another tool for better health management. If your sleep starts changing in concerning ways, especially if you’re acting out dreams or experiencing violent movements during sleep, it’s worth discussing with both your gastroenterologist and potentially a sleep specialist.
The Bottom Line
Your body is constantly communicating with you, sometimes in unexpected ways. If your sleep has been trying to tell you something about your IBD, now you have the science to back up those instincts. This research gives us permission to take our sleep seriously as part of our IBD management, not just as something nice to have when we can get it.
Remember, every breakthrough in IBD research brings us closer to better treatments and quality of life. This sleep connection might seem concerning at first, but it actually represents hope—another pathway to understanding and managing our condition more effectively. Trust your body’s signals, track what you can, and don’t hesitate to bring these observations to your medical team.
IBD Movement provides information for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.







